|
— endast 10 % av alla drabbade anses vara män, troligtvis p.g.a. felaktig diagnos — — män får i stället slentrianmässigt diagnosen kronisk prostatit —
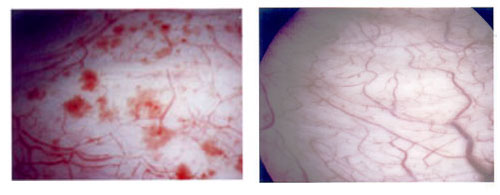
Allmänt om sjukdomen och symtom/symptom Interstitiell cystit/IC är en kronisk inflammation (utan bakteriella fynd) i urinblåsans vävnad och har vissa likheter (gemensamma orsaker?) med kronisk prostatit. På insidan av urinblåsan finns en ett epitelskikt/urothel som täcks av ett lager GAG/glycosaminoglycan, som skyddar urinblåsans vävnad mot de olika beståndsdelarna i urin. Vid IC är detta GAG-skikt skadat p.g.a. en immunologisk reaktion eller annan okänd orsak, vilket bl.a. innebär att olika kemiska ämnen i urin orsakar irritation eller mer eller mindre smärtsamma inflammationer i mer djupliggande vävnad. Vid cystoskopi kan man oftast konstatera att det finns glomerulationer (punktformiga spridda submucosa blödningar) eller mer eller mindre uttalade sårbildningar (ulcerationer) i urinblåsan.
Glomerulationer i urinblåsan Normal urinblåsa Hunners ulcer (sårbildning) i urinblåsan Bild från: http://www.urologkanalen.com Dr. Magnus Fall, Sahlgrenska Universitetssjukhuset
De vanligaste symtomen vid sjukdomen är:
Det tycks även vara vanligt att andra symtom förekommer tillsammans med den här sjukdomen. Enligt bl.a. en holländsk studie 1999 av Joop P van de Merwe M.D. PhD, Erasmus MC, Rotterdam är bl.a. följande sjukdomar vanligare bland drabbade av IC än genomsnittsbefolkningen: Allergier, fibromyalgi (led- och muskelvärk), colon irritabile (IBS), Crohns sjukdom/ulcerös colit, irritation i hud och slemhinnor, trötthet, SLE och Sjögrens syndrom. Se http://www.icpatienten.nl och http://www.essic.eu/associated_diseases.html Sjukdomen har varit känd sedan mitten av 1800-talet och det första symposiet om sjukdomen hölls 1987 av The National Institutes of Health i USA. Enligt internationella jämförelser, i första hand med en under 2005 publicerad finsk studie, uppskattar vi antalet drabbade (män och kvinnor) i Sverige till cirka 25 000 (prevalensen). Vi vill dock understryka, att det råder mycket stor osäkerhet om hur många som egentligen är drabbade. Vid en jämförelse med en amerikansk studie (totalt anses cirka 1,3 miljoner drabbade i USA, varav cirka 80 000 män) så skulle antalet röra sig om cirka 40 000. Cirka 90 % av de drabbade anses vara kvinnor, men troligtvis har många män fått diagnosen prostatit i stället för Interstiteill cystit? Studier i olika delar av världen anger allt från 10 drabbade per 100 000 till 850 drabbade per 100 000. Någon studie är oss veterligt inte gjord här i landet. Se även: http://www.wrongdiagnosis.com/i/interstitial_cystitis/stats-country.htm. The statistics used for prevalence/incidence of Interstitial cystitis are typically based on US, UK, Canadian or Australian prevalence or incidence statistics, which are then extrapolated using only the population of the other country. Från
AUA meeting 2005 har man presenterat följande siffror gällande USA: Det finns två former av sjukdomen. Den ena kallas för icke ulcerös interstitiell cystit och den andre för ulcerös (klassisk) interstitiell cystit. Den sistnämnda kallas även för "Hunner´s ulcers". Man räknar med att cirka 20 % av de som är drabbade har den här formen, som upptäcktes redan 1914 av Dr. Hunner. Denna karaktäriseras bl.a. av synbara (genom cystoskopi) sårbildningar i urinblåsan. Båda formerna ger oftast mer eller mindre spår av blod i urinen. I likhet med kronisk prostatit är orsaken till interstitiell cystit i de allra flesta fall okänd. Liksom kronisk prostatit anser man att det kan finnas flera olika orsaker till sjukdomen. Bakteriell, virologisk, immunologisk/autoimmun, neurologisk m.fl. Det är därför lätt att förstå varför den här sjukdomen är lika svår att diagnostisera, behandla och bota som kronisk prostatit. Olika källor anger att en statistisk genomsnittlig debut av sjukdomen ligger vid cirka 32 år. Andra källor anger att cirka 25 % är under 30 år då man utvecklar sjukdomen och att hälften av alla drabbade är över 40 år. Vid ett symposium hösten 2000 i USA, framkom att sjukdomen är vanligare bland barn än man trott. I de här fallen är andelen pojkar cirka 25 %. Man har bland annat konstaterat sjukdomen hos en 9 månaders baby, som varje gång grät av smärta innan hon urinerade. Enligt Dr. Susan F. Keay, M.D., Ph.D., Associate Professor of Medicine and Staff Physician at the Baltimore Veterans Affairs Medical Center (BVAMC), Baltimore, USA: "Interstitiell cystit är väldigt svårt att diagnosticera och ännu svårare att behandla. Sjukdomen är en ytterst smärtsam, långvarig och livsstillsförändrande sjukdom som kan bestå i många år."
Tillbaka till Appell till den svenska sjukvården
Olika hemsidor, diskussionsgrupper m.m. Under den här rubriken har jag lagt in länkar till olika patientföreningar och liknande runt om i världen: http://www.painful-bladder.org
-
International Painful Bladder Foundation (IPBF).
http://www.icforeningen.dk/index.html - Dansk IC förening. http://www.nofus.no/hjem.asp - Norsk urologisk förening http://www.niddk.nih.gov/health/urolog/pubs/cystitis/cystitis.htm - En bra hemsida om sjukdomen från NIH: http://www.b-p-s-a.org.uk - Bladder Pain Syndrome Association, UK. http://www.cobfoundation.org/index.html - The Cystitis and Overactive Bladder Foundation http://www.ic-network.com/world - International Patient IC Network. På hemsidan finns en omfattande information om det här nätverket och olika aktiviteter. http://www.ic-network.com - The Interstitial Cystitis Network. http://www.icpatienten.nl - the ICP, Interstitial Cystitis Patients’ Association in the Netherlands. http://www.ichelp.org - En mycket omfattande amerikansk hemsida. Grundad av Dr. Vicki Ratner. http://www.ic-hope.com/ - En hemsida av Catherine M. Simone "IC Hope for Interstitial Cystitis". Det finns en aktiv diskussionsgrupp för drabbade på denna hemsida. http://www.interstitialcystitis.co.uk - Engelsk hemsida.. http://webhome.idirect.com/e/espoir/ - Fransk hemsida. http://asso.orpha.net/AFCI/cgi-bin/ - Association Française de la Cystite Interstitielle http://usuarios.lycos.es/abatyci/ - Spansk hemsida http://www.ica-ev.de - Tysk hemsida. http://www.ica-austria.at - Österrikisk hemsida http://www.icsuccessonline.com - Amerikansk hemsida. http://www.gerohohlbrugger.at - En österrikisk urologs hemsida. http://www.essic.eu/criteria.html - ESSIC Classification Criteria Project Group http://luna.moonstar.com/~crc/ - Cystitis Research Center, Dr. Fuggazzotto. http://www.icsuccessonline.com/more_stories.htm - Lyckade behandlingsresultat.
Tillbaka till Information om ISOP
NIDDK Research Definition of Interstitial Cystitis Inclusion criteria: Glomerulations or Hunner's ulcer on cystoscopic examination, and Pain associated with the bladder or urinary urgency Exclusion criteria
Preliminära kriterier för IC/PBS enligt ESSIC/European Society for the Study of IC/PBS The ESSIC 2005 decided the following: Interstitial cystitis is PBS with typical cystoscopic and/or histological features in the absence of infection or other pathology; this definition differs from the ICS definition in the word and/or instead of and. [ICS definition 2002, modified ESSIC 2005]. This results in the following preliminary definition of IC/PBS: IC/Interstitial cystitis: Is a disease of unknown origin consisting of the complaint of suprapubic pain related to bladder filling, accompanied by other symptoms, such as increased daytime (>8x) and night-time (>1x) frequency, and with cystoscopic (glomerulations and/or Hunner's lesions) and/or histological features (mononuclear inflammatory cells including mast cell infiltration and granulation tissue) in the absence of infection or other pathology. PBS/Painful bladder syndrome: Is the complaint of suprapubic pain related to bladder filling, accompanied by other symptoms, such as increased daytime and night-time frequency, in the absence of proven urinary infection or other obvious pathology. This means that in the case of IC/PBS symptoms, the diagnosis of IC may be given if at least 1 of the objective "symptoms" is found. In other words, mast cells are not obligatory for the diagnosis of IC. http://www.essic.eu/criteria.html - ESSIC/European Society for the Study of IC/PBS. ESSIC is the European society for the study of IC/PBS: a scientific society of doctors/researchers, at the moment specifically working on a new definition of IC and new criteria for diagnosis. In 2005 chaired by professor Nordling in Denmark and Dr van de Merwe in the Netherlands is the project leader for the criteria project. Their aim is also to coordinate research etc. and share ideas. Enligt
http://www.uroweb.org
- The European Association of Urology (EAU):
Using the intersitital cystitis new diagnostic criteria in daily practice: About 156 patients Mouracade P, Lang H, Jacqmin D, Saussine C. Service d'urologie, hôpitaux universitaires de Strasbourg, 1, porte de l'Hôpital, 67091 Strasbourg, France. OBJECTIVES: To describe the characteristics of patients with interstitial cystitis and to determine what proportion of those patients met the European Society for the Study of interstitial cystitis/painful bladder syndrome 2005 (ESSIC IC/PBS) definition and how those who met the definition differed from those who did not. MATERIAL AND METHOD: A total of 156 patients diagnosed as having an interstitial cystitis were followed in our institution between 1997 and 2007. The diagnosis was suggested by the clinical history and confirmed on the basis of clinical symptoms, voiding diary findings, Pearson's test, O'Leary-Sant questionnaire, cystoscopy and hydrodistension and by the exclusion of other significant pathologies. The patients were evaluated in a prospective manner. We studied the demographics of our patients, described the common clinical presentation. We applied the ESSIC 2005 definition of CI/PBS on this population and found the proportion that meets this definition. RESULTS: The sex ratio F/M was 8:1. The patients were symptomatic for a median of 7.3 years before IC is diagnosed. The most common symptom was pain which was found in 100% of patients, frequency was found in 82% and nocturia in 62%. The common sites where pain was localized were suprapubic in 80%, perineal in 70% and genital in 40%. A burning sensation was found in 55% of patients. Hunner's lesion was found in three patients. The cystoscopy and hydrodistension revealed glomerulations in 88.4% of patients. The ESSIC 2005 definition identified only 74% of the 156 patients diagnosed as having IC/PBS. CONCLUSION: The symptoms in interstitial cystitis are variable. The ESSIC 2005 definition may not be sufficiently sensitive excluding over 26% of patients diagnosed as having IC. Minor modifications (pain type and location) of the definition appeared to increase its sensitivity.
Löpande information från International Painful Bladder Foundation, Nederländerna International Painful Bladder Foundation http://www.painful-bladder.org Faktablad http://www.painful-bladder.org/pdf/IPBF%20Publ%2006.pdf Kortfattad information http://www.painful-bladder.org/pdf/IPBF%20Publ%2005%20UK%20booklet.pdf Informationsbroschyr http://www.painful-bladder.org/pdf/Diagnosis&Treatment_IPBF.pdf
During the conference, 27 abstracts were presented on studies that directly or indirectly concerned PBS/IC with many of these presented in a dedicated moderated poster session on Infections/Inflammation of the Genitourinary Tract: Interstitial Cystitis (abstracts 111-136). A report on this conference including a review of all IC-related abstracts can be found on: http://www.painful-bladder.org/pdf/2007_AUA_Anaheim.pdf Webcasts from the AUA conference are available to browse through on: http://webcasts.prous.com/aua2007
Differences between Interstitial Cystitis/IC & Bacterial Cystitis/bakteriell cystit
Chronic, recurrent Urinary Tract Infections The December 2005 issue of Urology Times in an article on page 26-7 by Mac Overmyer quotes Scott Hultgren, Helen L. Stover Professor of Molecular Microbiology, at Washington University School of Medicine as saying, “According to his research, recurrent infections are probably more accurately described as resurgent infections because they evolve from quiescent reservoirs established not on the surface of bladder lumen, but in colonies within the umbrella cells of the bladder.”
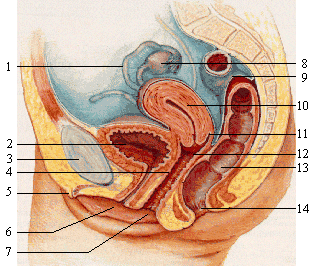
Int Urogynecol J. Pelvic Floor Dysfunct. 2006 Jan-Feb. Fitzgerald MP, Brensinger C, Brubaker L, Propert K; ICDB Study Group. Departments of Urology and Obstetrics and Gynecology, Loyola University Medical Center, Maywood, IL, USA. To describe the characteristics of pain experienced by patients with interstitial cystitis (IC) in terms of pain site, severity, and character, we performed a secondary analysis of data from the IC database (ICDB), which was a prospective, longitudinal, cohort study of IC patients. We analyzed the cross-sectional baseline data from 629 patients who had a completed baseline symptom questionnaire. Patients answered questions about whether they had pain or discomfort associated with urinary symptoms over the past 4 weeks and if so, about the location, characteristics, intensity, and frequency of their pain. Logistic regression examined associations between pain location and the presence of urinary symptoms. Analyses were performed using SAS version 8.2 (SAS Institute, Cary, NC, USA) and considered significant at the 5% level. Five hundred and eighty-nine (94%) patients with a mean age of 45 years (SD 14 years) reported baseline pain or discomfort associated with their urinary symptoms. The most common baseline pain site was lower abdominal (80%), with urethral (74%) and low back pain (65%) also commonly reported. The majority of patients described their pain as intermittent, regardless of the pain site. Most patients reported moderate pain intensity, across all pain sites. There was a statistically significant link between pain in the urethra, lower back, lower abdomen and urinary symptoms. PMID: 15995791 [PubMed - in process]
Interstitial cystitis: bladder pain and beyond Theoharides TC, Whitmore K, Stanford E, Moldwin R, O'Leary MP Tufts University School of Medicine, Department of Pharmacology and Experimental Therapeutics, Experimental Therapeutics 136 Harrison Avenue, Boston, MA 02111, USA. theoharis.theoharides@tufts.edu BACKGROUND: Interstitial cystitis is characterized by over 6 months of chronic pain, pressure and discomfort felt in the lower pelvis or bladder. It is often relieved with voiding, along with daytime frequency and nocturia in the absence of a urinary tract infection. Interstitial cystitis occurs primarily in females including adolescents and its diagnosis is still one of exclusion. It is now recognized as a serious medical condition associated with significant disability. OBJECTIVE: The aim of this paper was to review the pathogenesis and treatment of interstitial cystitis with emphasis on new pathogenetic trends and therapeutic modalities. METHODS: About 713 mostly original papers were reviewed in Medline from 1990 to August. 2008. All authors independently reviewed the literature. Large, double-blind, placebo-controlled, clinical trials were few and the medical histories of the patients used varied considerably making conclusions difficult. Promising pilot trials turned out mostly negative on follow-up. RESULTS: Increasing evidence of co-morbid diseases, neurogenic inflammation and the effect of stress are promising as new targets for pathophysiology. No new effective treatments have emerged. Oral pentosanpolysulfate, amitriptyline, hydroxyzine and quercetin, as well as intravesical heparin/bicarbonate/lidocaine solutions, are still used with variable success. Some pilot open-label trials presented encouraging findings. CONCLUSION: Interstitial cystitis contributes substantially to chronic pelvic pain and to poor quality of life. Oral or intravesical administration of solutions containing sodium hyaluronate, chondroitin sulfate and quercetin to both reduce bladder inflammation and 'replenish' the glycosaminoglycan layer should be tried. There is a clear need for therapeutic modalities. New potential translational research areas are suggested. PMID: 19006474 [PubMed - in process]
Sites of pain from interstitial cystitis/painful bladder syndrome. Warren JW, Langenberg P, Greenberg P, Diggs C, Jacobs S, Wesselmann U. Department of Medicine, School of Medicine, University of Maryland, Baltimore, Maryland 21201, USA. jwarren@medicine.umaryland.edu PURPOSE: In interstitial cystitis/painful bladder syndrome multiple pain sites are common. We hypothesized that a careful and systematic description of the pain of interstitial cystitis/painful bladder syndrome might provide clues to its pathogenesis. MATERIALS AND METHODS: Women with 12 months or greater of interstitial cystitis/painful bladder syndrome symptoms underwent a medical record review and interview. Each completed a questionnaire that included views of the female body and described up to 5 interstitial cystitis/painful bladder syndrome pains, noting 40 descriptors for each. RESULTS: Two-thirds of the 226 patients reported multiple pains. Pain could be consolidated at 4 sites, including suprapubic, urethral, genital and nongenitourinary. Most descriptors were similar and little evidence indicated that 1 pain influenced pain at another site. Another 3 patterns were evident, including 1) a suprapubic > urethral > genital > nongenitourinary ranking in site distribution and at each site proportions that were solitary, the worst and the most frequent pains, and pains that responded to bladder events, 2) site specific allodynia, and 3) for urethral and genital pains a wider spectrum of sensations, including burning, stinging and sharp. Patients with urethral (38%) or genital (27%) pain did not differ from those without such pain in 95% of 44 important characteristics. CONCLUSIONS: Suprapubic prominence and changes in the voiding cycle are features consistent with but do not prove that the bladder is the pain generator in interstitial cystitis/painful bladder syndrome and the pain sites described by patients are referred from it. The patients with interstitial cystitis/painful bladder syndrome who might have been diagnosed with vulvodynia or urethral syndrome did not differ from others in important patient variables. PMID: 18707715 [PubMed - indexed for MEDLINE]
Interstitial cystitis and other disorders Jag har hämtat följande intressanta citat från hemsidan hos den holländska gruppen Interstitial Cystitis Patients' Association of the Netherlands http://www.icpatienten.nl/ : "Certain facts are known about IC which give rise to the suspicion that it could be an autoimmune disease. IC is frequently associated with arthritis, systemic lupus erythematosus (SLE), thyroid disorders and Sjögren's syndrome. IC is often accompanied by joint pain, muscle pain, fatigue, gastrointestinal disorders, medicine intolerance, allergies, migraine, dry mouth, dry, irritated eyes, itchy, sensitive skin, vulvodynia and non-bacterial prostatitis".
Warren JW, Howard FM, Cross RK, Good JL, Weissman MM, Wesselmann U, Langenberg P, Greenberg P, Clauw DJ. Departments of Medicine, Epidemiology and Preventive Medicine, and Neurology, University of Maryland School of Medicine, Baltimore, Maryland, USA. OBJECTIVES: Probing for clues to the pathogenesis of interstitial cystitis/painful bladder syndrome (IC/PBS), we sought antecedent nonbladder syndromes that distinguished incident IC/PBS cases from matched controls. METHODS: Female incident IC/PBS cases were recruited nationally, and their IC/PBS onset date (index date) was established. The controls were recruited by national random digit dialing and matched to the cases by sex, age, region, and interval between the (assigned) index date and interview. The prevalence of 24 nonbladder syndromes before the index date was assessed, 7 by multiple methods. RESULTS: The cases with IC/PBS had greater antecedent prevalence of 11 syndromes, and 243 of 313 cases (78%) vs 145 of 313 controls (45%) had multiple syndromes (P < .001). Fibromyalgia-chronic widespread pain (FM-CWP), chronic fatigue syndrome, sicca syndrome, and irritable bowel syndrome were associated with each other by pairwise and factor analyses using numerous assumptions. Cases with FM-CWP, chronic fatigue syndrome, sicca syndrome, and/or irritable bowel syndrome (n = 141, 45%) were more likely to have other syndromes (ie, migraine, chronic pelvic pain, depression, and allergy). Three other syndrome clusters were identified; each was associated with this FM-CWP cluster. CONCLUSIONS: Eleven antecedent syndromes were more often diagnosed in those with IC/PBS, and most syndromes appeared in clusters. The most prominent cluster comprised FM-CWP, chronic fatigue syndrome, sicca syndrome, and irritable bowel syndrome; most of the other syndromes and identified clusters were associated with it. Among the hypotheses generated was that some patients with IC/PBS have a systemic syndrome and not one confined to the bladder.
Nonbladder related symptoms in patients with interstitial cystitis. J Urol 2001 Aug;166(2):557-61Erickson DR, Morgan KC, Ordille S, Keay SK, Xie SX. Department of Surgery, Division of Urology and Department of Health Evaluation Sciences, The Pennsylvania State University College of Medicine, Hershey, Pennsylvania, USA. PURPOSE: Clinical experience and epidemiological studies suggest that patients with interstitial cystitis have multiple nonbladder related symptoms. However, to our knowledge this finding has not been tested with a validated questionnaire and matched controls. With the University of Wisconsin scale, we compare the scores for patients with interstitial cystitis to those for control subjects. This validated questionnaire includes 7 bladder and 18 reference symptoms not related to the bladder. MATERIALS AND METHODS: A total of 35 female patients with interstitial cystitis and 35 age matched female controls completed the University of Wisconsin questionnaire. RESULTS: For the 7 bladder symptoms the difference between interstitial cystitis and control groups was extremely significant (p = 0.0001). Patients with interstitial cystitis had higher scores than controls for 2 reference symptoms, including other pelvic discomfort, backache, dizziness, chest pain, aches in joints, abdominal cramps, nausea, heart pounding and headache (p <0.01). However, they did not have higher scores for blind spots and/or blurred vision, numbness and/or tingling in fingers or toes, swollen ankles, feeling of suffocation, sore throat, cough, flu, nasal congestion and ringing in ears. The majority of patients with interstitial cystitis had a 0 score for all but 2 of the reference symptoms. CONCLUSIONS: Patients with interstitial cystitis had increased scores for 9 reference symptoms but did not indiscriminately report high scores for generalized complaints. This result suggests that in some cases of interstitial cystitis the pathophysiology may affect other organ systems besides the bladder. Alternatively, some of these symptoms may result from changes in sleep pattern or other factors associated with interstitial cystitis.
Department of Physiology, University of Oklahoma Health Sciences Center, 940 Stanton L. Young Boulevard, Oklahoma City, OK 73104, USA. Clinical observations of viscerovisceral referred pain in patients with gastrointestinal and genitourinary disorders suggest an overlap of neurohumoral mechanisms underlying both bowel and urinary bladder dysfunctions. Close proximity of visceral organs within the abdominal cavity complicates identification of the exact source of chronic pelvic pain, where it originates, and how it relocates with time. Cross-sensitization among pelvic structures may contribute to chronic pelvic pain of unknown etiology and involves convergent neural pathways of noxious stimulus transmission from two or more organs. Convergence of sensory information from discrete pelvic structures occurs at different levels of nervous system hierarchy including dorsal root ganglia, the spinal cord and the brain. The cell bodies of sensory neurons projecting to the colon, urinary bladder and male/female reproductive organs express a wide range of membrane receptors and synthesize many neurotransmitters and regulatory peptides. These substances are released from nerve terminals following enhanced neuronal excitability and may lead to the occurrence of neurogenic inflammation in the pelvis. Multiple factors including inflammation, nerve injury, ischemia, peripheral hyperalgesia, metabolic disorders and other pathological conditions dramatically alter the function of directly affected pelvic structures as well as organs located next to a damaged domain. Defining precise mechanisms of viscerovisceral cross-sensitization would have implications for the development of effective pharmacological therapies for the treatment of functional disorders with chronic pelvic pain such as irritable bowel syndrome and painful bladder syndrome. The complexity of overlapping neural pathways and possible mechanisms underlying pelvic organ crosstalk are analyzed in this review at both systemic and cellular levels. PMID: 17920206 [PubMed - as supplied by publisher]
Tuesday, 03 November 2009 BERKELEY, CA (UroToday.com) - Urologic and Non-urologic Unexplained Clinical Conditions OverlapUnexplained clinical conditions have been referred to by many names including functional somatic syndromes. They are characterized by a lack of clear physical or biological etiology, or inconsistent demonstration of laboratory abnormalities. Bladder pain syndrome and chronic pelvic pain syndrome (CPPS) in men NIDDK type 3 (nonbacterial prostatitis) would fall under this umbrella. Rodriguez and co-workers from Madrid, San Diego, and Seattle reviewed the literature on comorbidity between the most common urological pelvic pain syndromes (BPS, CPPS), vulvodynia, and the nonurological conditions of fibromyalgia, chronic fatigue syndrome, temporomandibular joint and muscle disorders, and irritable bowel syndrome. These conditions are characterized by symptoms such as pain, fatigue, sleep disturbances, and disability. The authors point out that the diagnosis often depends on the hallmark symptom and the expertise of the treating clinician rather than on the illness itself. They found 25 publications on comparison studies that provided data on the comorbidity of urological and nonurological unexplained clinical conditions or symptoms, 68% of which were published in the last 4 years! About 9% to 12% of patients with BPS also experienced fibromyalgia and 23-27% of patients with fibromyalgia also had symptoms consistent with BPS. Seven percent to 48% of patients with BPS or symptoms of BPS also had irritable bowel syndrome. Twenty-two percent of men with CPPS or its symptoms had irritable bowel syndrome. Thirty to 75% of individuals with BPS or BPS symptoms had irritable bowel syndrome in single condition studies, and 25%-56% of patients with irritable bowel syndrome had urinary problems. Likewise, 19%-79% of patients with CPPS had IBS or IBS symptoms. Of women with vulvar pain, 35% reported IBS. Studies of fibromyalgia, chronic fatigue syndrome, and temporomandibular joint pain suggest more modes comorbidity with urological syndromes. The
authors identified 3 dominant perspectives on the mechanisms of these
conditions: This
article is an excellent resource for providers interested in the gamut of
chronic unexplained pain conditions. Se: http://www.urotoday.com/index.php?option=com_content&task=view_ua&id=2225491
Från http://www.ub.gu.se/sok/dissdatabas/detaljvy.xml?id=3628 Dr. Ralph Peeker, Department of Urology ; Sahlgenska Universitetssjukhuset, Göteborg. Pressrelease: En studie visar att majoriteten av patienter med den såriga varianten av interstitiell cystit blir markant förbättrade om man hyvlar bort synliga sår. Detta kan göras med ett instrument som förs in via urinröret. Ingreppet äger rum antingen i narkos eller i ryggbedövning och kräver i genomsnitt tre dagars vårdtid. Interstitiell cystit är en sjukdom som drabbar urinblåsan som innebär svår smärta vid blåsfyllnad samt täta trängningar till vattenkastning, ibland upp emot etthundra gånger per dygn. Sjukdomen sträcker sig oftast över decennier och hör till de mest plågsamma tillstånd som förekommer inom urologin. Interstitiell cystit leder till låg livskvalitet, långa sjukskrivningsperioder och sjukpensionering, ökat antal självmord samt frekvent och kostsamt omhändertagande i sjukvården med stor och ibland stympande kirurgi och krav på livslång uppföljning. Även om sjukdomen varit känd i över hundra år vet man inte vad den beror på och man känner inte heller till uppkomstmekanismens olika steg. Det är dock sedan tidigare känt att interstitiell cystit yttrar sig såsom två olika former: en form där man har synliga sår i urinblåsan och en form som saknar sår. På vissa patienter med den såriga varianten skrumpnar urinblåsan ihop nästan helt och då hjälper det inte att hyvla. Man kan istället operera bort större delen av urinblåsan och ersätta den med tarm. Studien visar att patienter med den såriga varianten blir besvärsfria efter denna operation. Detta omfattande ingrepp hjälpte dock ej alls patienterna som hade den ickesåriga formen av sjukdomen. Avhandlingen visar också att en särskild cell, som benämnes mastcell och som sedan länge är känd för att vara inblandad vid olika typer av inflammation, verkar vara av stor betydelse för sjukdomsutvecklingen vid den såriga formen av interstitiell cystit. Studien påvisar också två ämnen som troligen kan stimulera mastcellerna vilket i sin tur kan orsaka de svåra symptomen vid sjukdomen. Vidare forskning i den här riktningen bör kunna klarlägga de bakomliggande sjukdomsmekanismerna och därigenom göra det möjligt att skräddarsy verkningsfulla mediciner. På så vis skulle man kunna hjälpa många patienter ur en socialt handikappande tillvaro.
Report on the 2nd International Consultation on Interstitial Cystitis, Japan 2007
Written by Philip M. Hanno, MD. Thursday, 10 May 2007. Dr. Leroy Nyberg from the National Institutes of Health concluded the meeting with a new paradigm that the NIDDK may determine as the foundation of future research studies, considering Painful Bladder Syndrome/Interstitial Cystitis/Bladder Pain Syndrome as a bladder manifestation of a more global disorder that can result in one of a number of pain or inflammatory syndromes; witness the large number of disorders found to be associated with BPS/IC. Från UroToday.
Leroy Nyberg MD, speaking in Kyoto on behalf of the NIDDK, announced that the NIDDK had decided to take an entirely new approach to the study of IC since research so far has not led to any breakthrough in finding adequate treatment for the disease. According to Dr Nyberg, there is a need to change gear and the NIDDK will therefore hold a meeting in the autumn of 2007 to re-define the research definition. They plan to make the research definition less “bladdercentric”and make it more patient-centric and more holistic, focusing on IC as a systemic disease, with manifestations in the bladder, but also elsewhere in the body and will involve doctors from various disciplines, including international experts.
Prevalence of Painful Bladder Syndrome in Older Women Lifford KL, Curhan GC Channing Laboratory, Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts; Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts. OBJECTIVES: To examine the prevalence of and symptoms associated with painful bladder syndrome (PBS) in a population of older women, utilizing the Nurses' Health Study (NHS) cohort. METHODS: In 2004, NHS participants were asked by mailed questionnaire, "In the past 10 years, have you experienced bladder or pelvic pain associated with urinary symptoms for more than 3 consecutive months?" Women who responded "yes" were sent a detailed supplementary questionnaire. A severity score was calculated according to information about symptoms and bother in the previous 6 months. RESULTS: The PBS screening question was answered by 67,095 participants. A supplemental questionnaire was sent to all 4005 women who answered yes, and 3042 (76%) responded. Symptoms consistent with PBS were reported by 1548 respondents (51%), representing 2.3% of the screened cohort. The prevalence of PBS was 1.7% in those younger than 65 years and increased progressively to 4.0% in women aged 80 years and older (P trend <0.001). Severity, based on both symptoms and bother, was mild in 14.8% of women with PBS, moderate in 29.0%, and severe in 56.2%. CONCLUSIONS: Painful bladder syndrome is a common condition in women. The prevalence of PBS increases with age, and the vast majority of women with PBS have moderate or severe symptoms.
Keep an eye out for Interstitial Cystitis in male patients Urology Times March 1998 Ten percent of interstitial cystitis (IC) cases are men, but it is often all to easy for urologists to miss the diagnosis. Instead, patients are treated for nonbacterial prostatitis or prostatdynia, "and they don't get better", according to Grannum R. Sant, MD, professor and chairman of urology at Tufts University School of Medicine, Boston, who spoke at the International Research Symposium on Interstitial Cystitis. "Bladder pain is misdiagnosed as prostate pain because of the anatomic proximity of both organs". If the patient has symptoms of prostatitis and you've ruled out bacterial prostatitis, treat them for non-bacterial prostatitis or prostatdynia. If they do not get better, cystoscopy is recommended. Think IC when your patient with prostatitis is not getting better”. “We must break down the difference between the urologist, the gynaecologist, the gastroenterologist and treat the pelvic floor as a single unit".
Chronic Prostatitis Symptoms May Be Due to Bladder Pathology BJU Int 2005; 95: 86-90. BERKELEY, CA (UroToday Inc.) - Patients with chronic prostatitis and interstitial cystitis can be the some of the most difficult patients to diagnose and treat. There is some speculation that the two diseases may be closely connected. Dr Parsons and colleagues from San Diego and LaJolla, CA and Jackson, MI performed a study to determine whether men diagnosed with "prostatitis" have pathology originating within the bladder, and whether the pelvic pain and urgency/frequency (PUF) questionnaire correlates to results of the potassium sensitivity test (PST). They also performed a study to see the effects of KCl irrigation on the urethra. Their results were published the January 2005 edition of BJU International. Fifty men with prostatitis recruited from urologic or primary care offices, who were treated with at least one course of antibiotics, completed a PUF questionnaire and had a PST. There were 14 controls who also completed the PUF questionnaire and underwent a PST. Patients with prostatitis had significantly higher PUF scores ( 7 in the prostatitis group but 1 in the controls). None of the controls had a positive PST while 77% of the prostatitis patients had a positive PST. In a separate group, 22 male controls had their urethra irrigated with KCL and rinsed and were asked to rate any urgency or pain. The urethras were then irrigated with protamine sulphate, which disrupts the barrier function of the urothelium. Half the men then underwent urethral irrigation with 0.2 mol/L KCl while the other half underwent urethral irrigation with 0.2mol/L NaCl. They were then asked again to rate their urgency and pain. All 11 who had a repeat irrigation with KCl reported pain and four had urgency. None of the men irrigated with NaCl reported pain and 2 reported urgency. The authors conclude that men diagnosed with prostatitis may have pathology originating from the bladder and that this situation is partially responsible for their symptoms. This adds to the idea that IC and prostatitis may be more closely linked than originally thought. The PUF score also appears to be a strong predictor of PST outcome. In addition the findings of urethral pain after mucosal injury suggest that urethral symptoms can arise from abnormal urothelial permeability and potassium cycling.
Summation Model of Pelvic Pain in Interstitial Cystitis - Abstract Departments of Urology and Microbiology-Immunology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA. d-klumpp@northwestern.edu. Many patients with interstitial cystitis (IC) find that particular foods exacerbate disease symptoms. These patients may modify their diet to manage symptoms, but the mechanism by which dietary modification benefits patients with IC is unclear. We hypothesize that integration of neural signals from pelvic organs mediates the effects of diet on symptoms of IC. In animal models, pelvic inflammation is subject to crosstalk, so an inflammatory stimulus in one pelvic organ evokes a response in an independent organ..Recent data show that the colon can modulate bladder-associated pelvic pain in mice. As pelvic organs are innervated through shared circuitry, perceived pelvic pain might occur when spatial summation of individual pelvic inputs exceeds a threshold. Through this mechanism, a noxious dietary stimulus, which otherwise does not exceed the pain threshold in a normal individual, may substantially exacerbate pain in a patient with bladder symptoms. Repeated painful stimuli over time further contribute to symptoms by a process of temporal summation, resulting in enhanced responsiveness through central sensitization. Thus, pelvic organ crosstalk might modulate symptoms of pelvic pain by spatial and temporal summation, suggesting a mechanism for the benefits of dietary modification in patients with IC, as well as therapeutic opportunities.
Observations on the presentation, diagnosis, and treatment of interstitial cystitis in men. Urology 2001 Jun;57(6 Suppl 1):26-29 Forrest JB, Vo Q. Urologic Specialists of Oklahoma, Inc., Tulsa, Oklahoma, USA. This article presents and evaluates the symptoms, presentation, diagnosis, and treatment of men with interstitial cystitis (IC). A retrospective chart review and an interview of all men in our practice diagnosed with IC since 1990 was performed. The patients' presenting symptoms, physical findings, clinical evaluation, and responses to therapy were reviewed. A total of 52 men were identified during the study who met the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) criteria for diagnosis of IC. The most common referral diagnosis was prostatitis with the most common predominant symptoms being suprapubic pain with urinary frequency and dysuria. A significant number of male patients also developed sexual dysfunction. All patients met the NIDDK criteria for a diagnosis of IC. Multiple therapies were used for the treatment of these patients over the study period. Five patients were initially treated with dimethyl sulfoxide (DMSO) as a sole agent; however, all intravesically treated patients eventually failed this form of therapy. A total of 37 of 52 patients were treated with multidrug oral therapy. Findings showed that 80% of patients achieved >75% improvement in their symptomology at 6 months of follow-up with a durable response at 1 year. IC in men is probably underdiagnosed and is most commonly misdiagnosed as prostatitis. The patient's presentation is analogous to that in the female population allowing for gender differences. The patients responded well to multidrug oral therapy.
Differences between CPPS and male IC Urology. 2004 Jan;63(1):22-6. Antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor in men with interstitial cystitis versus chronic pelvic pain syndrome. Keay S, Zhang CO, Chai T, Warren J, Koch K, Grkovic D, Colville H, Alexander R. Division of Infectious Diseases, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, USA. OBJECTIVES: To determine whether men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) have urine markers previously described for patients with interstitial cystitis (IC; presence of antiproliferative factor [APF] activity, decreased levels of heparin-binding epidermal growth factor-like growth factor [HB-EGF], and increased levels of epidermal growth factor). METHODS: Clean catch urine specimens were collected from 41 symptomatic patients with CP/CPPS, 36 asymptomatic men without bladder disease who served as the control group, and 24 men with IC. APF activity was determined by (3)H-thymidine incorporation into primary normal adult human bladder epithelial cells. HB-EGF and epidermal growth factor levels were determined by enzyme-linked immunosorbent assay. RESULTS: Men with CP/CPPS did not differ significantly from asymptomatic controls for any of the three markers tested (P >0.49). In contrast, APF activity was present significantly more often and HB-EGF levels were significantly lower in the urine specimens from men with IC than in the specimens from controls or patients with CP/CPPS (P <0.00001 for all four comparisons). Although the epidermal growth factor levels also tended to be higher in the urine from patients with IC than in the urine from controls, the difference did not reach statistical significance (P = 0.06). CONCLUSIONS: These findings indicate that at least two of the urine biomarkers previously identified in women with IC (presence of APF activity and decreased levels of HB-EGF) are also found in men with IC, but not in men with CP/CPPS. This finding suggests that IC and CP/CPPS may be two different disorders with distinct pathophysiologies. It also confirms the utility of the presence of APF activity and HB-EGF levels as markers for IC in men, as well as in women, with this disorder.
Interstitial cystitis: current issues and controversies in diagnosis. Urology [the Gold Journal] 2001 Jun;57(6 Suppl 1):82-8. Sant GR, Hanno PM. Department of Urology, Tufts University School of Medicine, Interstitial Cystitis Center, New England Medical Center, Boston, Massachusetts 02111, USA. Mail: gsant@lifespan.org Up to 70% of men with symptoms of nonbacterial prostatitis and prostatodynia have the cystoscopic appearance (NIH-NIDDK criteria) of IC when cystoscoped under anesthesia.[34 and 35] This raises the possibility that IC in men frequently masquerades as nonbacterial prostatitis/prostatodynia. The recent classification of the type 3 prostatitis syndrome as chronic pelvic pain syndrome (inflammatory and noninflammatory) suggests that IC and chronic bacterial prostatitis/prostatodynia may be the same syndrome. [34 and 35] The symptoms in both conditions are similar, including irritative voiding symptoms, pain (pelvic, bladder, prostate, genital), sexual dysfunction, and the comorbidities of depression and anxiety. In a pilot open-label study, sodium pentosan polysulfate (a drug used to treat IC) reduced the severity and frequency of voiding symptoms and pain, and improved the quality of life in men with the chronic pelvic pain syndrome. [36]. CPP may be the primary symptom of IC. Such patients with bladder pain, dyspareunia, and perimenstrual symptom exacerbation are frequently referred for gynecologic evaluation whereas patients with bladder irritability present to urologists and gynecologists with symptoms of the overactive bladder and are treated with oral anticholinergics. IC is a common cause of CPP in women.[11 and 37] A significant percentage of women with CPP remain undiagnosed after full gynecologic evaluation. Laparoscopic evaluation in this group of patients is negative or reveals microscopic endometriosis. These data strongly suggest that gynecologists, urogynecologists, and primary care physicians need to consider IC in the differential diagnosis of CPP in women.
Diagnos av interstitiell cystit På diskussionsgrupp sci.med prostate.prostatitis den 29 juni 2001, skriver Dr. Dimitrakov bl.a. följande. IC can be diagnosed in one of three ways: 1) Presence of APF (anti-proliferative factor) and glycoprotein-51 in the urine - available at the academic setting only. Sensitivity and specificy - 95 %. 2) Potassium sensitivity test (infuse potassium solution) - specificty 60 % 3) Cystoscopy with hydrodistension
Bakteriologisk diagnostik vid IC Om bakteriologisk diagnostik se rubriken Diagnostic Test Philosophy (IC) på sidan Bakteriologisk diagnostik vid urogenitala sjukdomar.
Diagnos av interstitiell cystit enligt SUF/Svensk Urologisk FöreningDiagnosen interstitiell cystit måste ställas med endoskopi, och då krävs det att patienten är sövd eller fått någon annan form av komplett bedövning. Urinblåsan utvidgas med 70–80 cm pålagt vattentryck tills den maximala blåsfyllnaden uppnåtts. Utseendet på blåsans slemhinna före och under utvidgningen registreras noggrant. De viktigaste observationerna görs när man granskar blåsslemhinnan efter utvidgningen. De förändringar som man anser bevisa sjukdomen framträder först då. Två former av förändringar kan observeras: Vid den klassiska formen finns det rodnade områden i blåsan, ett eller flera, med små, fina kärl som är radiärt anordnade mot centrum av lesionen, där man kan se ett blekt ärr, en liten fibrintofs eller ett koagel. Mitt i en sådan förändring brister slemhinnan när blåsan spänns ut. Rupturen löper ned i submucosan, med sivande blödning från små kärl i ärrets botten och slemhinnekanterna (Fall, Johansson, Aldenborg 1987, 62). Ett mer eller mindre framträdande slemhinneödem finns runt förändringen. Den andra typen av förändring som också betraktas som interstitiell cystit har ett annorlunda utseende. Slemhinnan ter sig normal innan blåsan utvidgas. Under utvidgningen kan små, mycket tätt ställda och ytliga slemhinnefissurer utvecklas, så att ett gatstensliknande mönster framträder. Efter utvidgningen kan man se en tät utsådd av punktformiga, mycket små submucösa blödningar, så kallade glomerulations, praktiskt taget överallt. Denna form av sjukdomen kallas non-ulcerös interstitiell cystit. En biopsi ger vägledning om diagnosen och subklassificeringen av sjukdomen (Fall, Johansson, Aldenborg 1987, 62). Förutom att det är önskvärt att bekräfta förekomsten av mastceller, lymfocyter och plasmaceller samt urothelets tillstånd, tjänar biopsin ytterligare ett viktigt syfte. Vid cystoskopisk undersökning kan det ibland vara svårt att skilja blåssjukdomar som tuberkulös cystit och carcinoma in situ från interstitiell cystit, liksom andra mera ovanliga former av kronisk cystit.
Svensk Urologisk Förenings hemsida finns på http://www.urologi.org
Interstitiell cystit, molekylärbiologiska studier Skapat av: Yr Logadottir, Sahlgrenska Universitetssjukhuset i Göteborg 2008-09-23 Interstitiell cystit (IC) är en kronisk invalidiserande sjukdom i urinblåsan. Etiologien till IC är ej känd. IC finns i två presentationer, klassisk och nonulcerös. Sjukdomen kännetecknas av svåra smärtor vid fyllnad av urinblåsan, som lättar vid tömning, vilket leder till starkt ökat antal toalettbesök natt och dag. Symptomen är desamma för de två presentationerna. Skillnaden är att sluttstadiet för klassisk IC är en skrumpblåsa pga destruktiv inflammation som ofta nödvändiggör avancerad rekonstruktiv kirurgi. Könsfördelningen är 10:1 kvinnor:män. För diagnos behöver patienten bl a undersökas i narkos med distension av urinblåsan, granskning av förändringar p.g.a. distension samt provtagning från blåsslemhinnan. Vår
forskningsgrupp har påvisat att klassisk och nonulcerös IC representerar olika
sjukdomar. Klassisk IC är en äkta inflammatorisk sjukdom medan nonulcerös IC
saknar tydliga inflammationstecken. Klassisk IC har bland många andra särdrag
en dramatiskt hög frisättning av kväveoxid (NO) från blåsväggen samt
markant infiltration av mastceller i blåsväggen inklusive slemhinnan. Vi anser
bl.a. undersöka vilka celler som producerar NO och vilken isoform av enzymet kväveoxidsynthas
(NOS) som är involverad. En ytterligare frågeställning är vilka olika
inflammationsmarkörer som är relevanta. Tillgängliga data pekar på att vissa
sådana torde vara mera intressanta, t.ex. TNF (Tumour Necrosis Factor), vissa
interleukiner och cytokiner, samt tillväxtfaktorer som IGF-binding protein-3
och interleukin-6. Speciell uppmärksamhet har riktats mot epitelförändringen
vid interstitiell cystit och faktorn APF (Anti Proliferative Factor). Målsättningen är att förbättra diagnostiken av en mycket plågsam sjukdom, den mest plågsamma benigna sjukdomen som drabbar urinblåsan, samt att analysera den specifika inflammationen vid klassik IC för att få en inblick i skeenden i inflammtionskaskaden. Förbättrad diagnostik kommer att leda till effektivare utvärdering av olika behandlingsalternativ och förhoppningsvis i förlängningen skapa ett fundament för att kunna behandla sjukdomen rationellt, kausalt, farmakologiskt. Se http://www.fou.nu/is/sverige/document/12161
Ueda T, Nakagawa M, Okamura M, Tanoue H, Yoshida H, Yoshimura N Department of Urology, Kyoto City Hospital, Kyoto, Japan. Objectives: Diagnosing the bladder lesions associated with interstitial cystitis/painful bladder syndrome (IC/PBS) is sometimes difficult for general urologists. We therefore aimed to develop an IC/PBS diagnosis method using a cystoscope with a narrow-band imaging (NBI) system that can detect mucosal angiogenic lesions. Methods: Fifty-two subjects suspected of having IC between October 2006 and June 2007 were included in this study. There were 49 women and three men, ranging in age from 19 through 85 with an average age of 59. First, conventional cystoscopy under spinal anesthesia was performed to examine the ulcerative lesions by a urological specialist. Then, other health care professionals made a separate observation of capillary-rich areas of the superficial layer of the bladder mucosa by cystoscopy with the NBI system. Results: Among the 52 patients, 37 cases were found to have ulcers by conventional cystoscopy, which were also recognized as capillary-rich brownish areas using the NBI system (100% accuracy); 13 cases were found to have NBI-positive areas without ulcer, which were coincided with those with petechial hemorrhages and glomerulations following subsequent hydrodistention; and two cases of normal mucosa were detected. Furthermore, six cases of bladder cancer (carcinoma in situ) were detected by biopsies that were obtained from the ulcerative lesions positively identified by NBI cystoscopy. Conclusions: Examining the urinary bladder mucosa with a flexible cystoscope with the NBI system makes it possible to easily detect ulcers of bladder mucosa and areas with angiogenesis. Therefore, it is considered that the use of a flexible cystoscope with the NBI system is highly practical for the IC/PBS diagnosis.
Nitric oxide - A useful marker in the diagnosis of lower urinary tract disorders, Sverige Ingrid Ehren*, Abolfazl Hosseini, Peter N Wiklund, Stockholm, Sweden Introduction and Objectives: Lower urinary tract symptoms as urgency, frequency, nocturia and pain are very common symptoms in patients referred to urologists. The aim of this study was to investigate if measurement of luminal nitric oxide (NO) in the urinary bladder can be used to differentiate patients with inflammation in the urinary bladder from patients with non-inflammatory disorders causing these symptoms. NO is produced by the mucosa in hollow organs and it has previously been shown that the NO concentration is elevated in inflammatory disorders in both the airways and the intestine. Methods: The NO production in the urinary bladder was measured by introducing a silicon catheter into the bladder and 25 mL of room air was infused into the catheter balloon. After 5 min. of incubation, the air was aspirated and analyzed with chemiluminescense technique and the peak levels of NO were registered. Patients with urgency due to interstitial cystitis (n=18), bacterial cystitis (n=6), irradiation cystitis (n=5), BCG-induced cystitis (n=17), detrusor instability (n=9), outflow obstruction (n=8), sensory urge (n=22) and patients with superficial bladder cancer (n=19) and carcinoma in situ (n=9) were examined. Patients with stress incontinence were used as controls (n=16). Reagent strip analysis was positive in the group with infections but negative in all other patients. Results: The NO concentration was markedly increased in patients with interstitial cystitis (327±210 parts per billion (ppb), (mean ± SEM), bacterial cystitis (896±282 ppb), irradiation cystitis (633±540 ppb) and BCG-induced cystitis (510±313 ppb) as compared to the patients with detrusor instability (11±1 ppb), outflow obstruction (9±1 ppb), sensory urge (10±1 ppb) and controls (13±2 ppb). In patients with superficial bladder tumor the NO concentration was also low, 3±1 ppb while it was slightly increased in patients with carcinoma in situ , 23±9 ppb. Conclusions: Measurement of NO in air from the urinary bladder is a safe, fast method to diagnose inflammatory disorders in the urinary bladder and the simplicity of the method makes it potentially useful as a screening method for office use. Se även http://www.aerocrine.se/swedish/no_clinical_bladder.html
Scientists discover toxin that may be key to diagnosing, treating mysterious ailment By Lauran Neergaard, Associated Press Tuesday, March 25, 2003 - WASHINGTON -- The stabbing pain started overnight, like bolts of electricity shooting through Kristina Hinchliff's pelvis. She had to race to the bathroom every 15 minutes, night and day. It took a year of visits to emergency rooms and numerous physicians to find the answer: Hinchliff has a debilitating type of bladder inflammation that afflicts a million Americans yet baffles doctors. There is no test for this disease, called interstitial cystitis, and no cure. While there are treatments to ease the symptoms, they don't help everyone. Specialists hope that's about to change: Scientists have discovered IC patients harbor a toxin in their bladders that might prove key to understanding -- and quickly diagnosing -- the ailment. At the same time, studies of some promising treatments are under way. "It is a very exciting period," says Dr. Josephine Briggs, who oversees urology research at the National Institutes of Health. IC is a chronic inflammation of the bladder that strikes mostly younger women. It leaves the organ's lining bleeding, scarred, and unable to hold normal amounts of urine. While IC strikes with varying severity, some patients must urinate once an hour, even more, every day for years, and can suffer unrelenting pain. The Social Security Administration just ruled IC incapacitating enough to render someone legally disabled. No one knows what causes IC. Many doctors didn't even recognize it as a disease: Dr. Vicki Ratner founded the patient-advocacy Interstitial Cystitis Association in the 1980s after becoming ill in medical school and having 14 doctors say it was all in her head. Even today, diagnosis is made by ruling out everything else and then putting the patient under general anesthesia to stretch the bladder wall in search of some hallmark signs. A discovery by Dr. Susan Keay at the University of Maryland may help. Keay found that the bladder cells of IC patients churn out a toxin called APF, or antiproliferative factor. APF appears to decrease levels of a growth factor, called HB-EGF, that's important in producing cells necessary to repair a damaged bladder lining. This spurs a vicious cycle where the bladder harms itself and then blocks its own healing mechanisms. Measuring these two compounds in urine is laborious, and for now experimental. Keay is talking with several companies about creating easier tests that doctors might one day offer. But the discovery could prove far more crucial, says Monica Liebert, the American Urological Association's research director. Not only does it point to a possible root cause of IC, but it suggests that bladder growth factor might be used as a treatment -- a next step to be explored if Keay's research is ultimately proven. Specialists are anxiously watching two other potential treatments much farther in development: - BCG is a bacterium used as a tuberculosis vaccine and to treat bladder cancer. When infused directly into the bladder, it seems to cause cells in the bladder lining to die and new ones to grow -- a process that can itself cause severe pain. Results of testing on 260 patients given either BCG or a dummy infusion are expected next year. - ICOS Corp. is beginning a study of a drug called RTX that promises to deaden certain bladder nerves believed integral to IC symptoms. Scientists also are considering studying if botulinum toxin -- sold as a wrinkle-reliever under the name Botox -- might help by temporarily paralyzing some bladder nerves. For now, some treatments do offer many people relief. They range from painkillers, including narcotics, to infusing more powerful drugs, including heparin and the solvent DMSO, directly into the bladder using a catheter. But it's still a hurdle to find a doctor who knows all the options -- and understands that IC warrants such major treatment as narcotics, says Hinchliff. The 30-year-old Portland, Ore., woman finally found a specialist through the Interstitial Cystitis Association. "One of the hard things about IC is that it's invisible. ... We look totally normal," she said. "It's just started to be on the map."
De preparat/behandlingar som f.n. står till förfogande är:
Andra behandlingsmodeller är:
I de fall då preparat inte är godkända för bruk i Sverige har läkare möjlighet att ansöka om tillstånd att använda dessa genom en licensansökan. Denna skall lämnas till Apotek för vidare handläggning.
Treatment of bladder pain syndrome/interstitial cystitis 2008: can we make evidence-based decisions? Dr. M. Fall, Dr. F Oberpenning, Dr. Ralph Peeker. Department of Urology, Sahlgrenska Academy, Göteborg University, Göteborg, Sweden. magnus.fall@urology.gu.se CONTEXT: Opinions on how to best treat bladder pain/interstitial cystitis are ambiguous. OBJECTIVE: To review previous and recent literature on this subject to assess the current state of evidence. EVIDENCE ACQUISITION: With important previous papers reviewed for the 2003 European Association of Urology guidelines as background, the PubMed database was searched and articles published in 2003-2007 were reviewed and relevant ones were selected for detailed study. EVIDENCE SYNTHESIS: A large number of studies describing a variety of quite dissimilar therapeutic principles were retrieved. The various methods and level of evidence are summarised in tables. Only pentosan polysulfate sodium (oral and intravesical), amitriptyline, hydroxyzine, cyclosporin A, intravesical dimethyl sulfoxide, transurethral resection of visible Hunner lesions, and major reconstructive surgery reached a high degree of recommendation. However, a number of pitfalls hamper evaluation of the available information; a crucial one is that our understanding of basic mechanisms causing bladder pain is fragmentary. So far, we are faced with a large variety of hypotheses although it is difficult to identify the most relevant ones. In this respect, we are not much helped by the recent literature because many studies have poor descriptions of patients or are of a pilot character, with no follow-up by larger trials. Controlled studies are rather scarce. On the other hand, some good-quality studies following up positive pilot trials end up with negative results. CONCLUSION: Perhaps the most significant problem concerns inclusion and exclusion criteria in bladder pain syndrome/interstitial cystitis studies. At this stage, it is not too easy to communicate the wide available expert knowledge to the general audience. More sophisticated standards, capable of being generally used, have to come. PMID: 18403099 [PubMed - in process]
Daha LK, Riedl CR, Lazar D, Simak R, Pfluger H. Department of Urology and Ludwig Boltzmann Institute of Urology and Andrology, Municipal Hospital Hietzing, Vienna, Austria. Objective: To evaluate changes in bladder capacity and potassium sensitivity after glycosaminoglycan (GAG) substitution therapy. Material and methods: The study population comprised two groups of female patients with bladder pain syndrome/interstitial cystitis (BPS/IC): responders (those with symptom improvement) and non-responders (those without symptom improvement) after a 10-week period of intravesical, episodic, weekly, GAG substitution therapy. A total of 27 volunteers with increased pre-therapeutic potassium sensitivity were enrolled in the study and re-evaluated using the modified comparative potassium test (maximal bladder capacity with a saline solution versus a 0.2 M KCl solution) following intravesical GAG substitution therapy. Results: In the 13 responders, the average maximal bladder capacity increased by 17% with the saline solution and by 101.5% with the 0.2 M KCl solution. In the 14 non-responders, post-therapeutic average maximal bladder capacity was decreased by 35% with the saline solution and remained relatively unchanged after instillation with a 0.2 M KCl solution. Conclusion: These data demonstrate that in patients who respond symptomatically to intravesical GAG substitution therapy, cystometric bladder capacity is increased, whereas non-responders experience a decrease in bladder capacity. Från http://www.urotoday.com/index.php?option=com_content&task=view_ua&id=2218156
Interstitial cystitis relieved by heparin and lidocaine Reuters Health Posting Date: February 18, 2005. NEW YORK (Reuters Health) - In patients with interstitial cystitis, intravesical administration of a combination of heparin and alkalinized lidocaine immediately reduces symptoms and can serve as a therapeutic bridge during the months until traditional heparinoid treatment reaches its full effect. While heparinoid-based therapy is effective against interstitial cystitis, it often takes several months or more of treatment before pain and feelings of urgency are relieved, Dr. C. Lowell Parsons of the University of California, San Diego Medical notes. Intravesical agents have been used in the past as adjunctive treatments, but even heparin, one of the most widely used, is effectively in only about 50% of patients. In 82 patients with newly diagnosed interstitial cystitis, Dr. Parsons instilled a solution of 40,000 units of heparin, 3 mL 8.4% sodium bicarbonate, and 8 mL of 1% lidocaine (80 mg) or 2% lidocaine (160 mg). On the Patient Overall Rating of Improvement of Symptoms scale, significant immediate symptom relief was reported within 20 minutes of intravesical administration by 35 of 47 patients treated with 1% lidocaine and by 33 of 35 treated with 2% lidocaine, according to Dr. Parsons' report, published in the January issue of Urology. Among the patients who received the higher dose, 50% had at least 4 hours of relief from a single instillation, and several had relief lasting as long as 48 hours. Of 20 patients who elected to receive additional instillations, 16 had sustained significant relief after 2 weeks of treatment. "Because it produces symptom relief for hours beyond the period of immediate anesthetic effect of the lidocaine, the solution appears to downregulate bladder sensory nerves past the actual anesthetic period and thus may accelerate the recovery of the bladder," Dr. Parsons writes. The researcher points out that the sodium bicarbonate alkalinizes the solution and increases the absorption of lidocaine. "The 1% lidocaine solution should be tried first," Dr. Parsons advises. "If it does not produce symptom relief in the patient, the amount can be increased safely to 8 mL of 2% lidocaine." "The development of this solution," Dr. Parsons concludes, "may represent a significant advance both in the treatment of interstitial cystitis and in the understanding of the downregulation of sensory nerves." Urology 2005;65:45-48.
Nickel JC, Moldwin R, Lee S, Davis EL, Henry RA, Wyllie MG North Shore Long Island Jewish Health, Hyde Park, NY. OBJECTIVE: To assess the immediate and sustained relief of the symptoms of interstitial cystitis/painful bladder syndrome (IC/PBlS) after a consecutive 5-day course of treatment with intravesical alkalinized lidocaine (PSD597), and to characterize the pharmacokinetics of single and multiple doses of intravesical PSD597 in a subgroup of patients. PATIENTS AND METHODS: In all, 102 adult patients (99 women) with a clinical diagnosis of IC/PBlS were randomized from 19 centres in the USA and Canada to receive a daily intravesical instillation of PSD597 (200 mg lidocaine, alkalinized with a sequential instillation of 8.4% sodium bicarbonate solution, to a final volume of 10 mL) or placebo (double-blind), for 5 consecutive days. Patients were followed at intervals up to 29 days after the first instillation. Efficacy was assessed by changes in the Global Response Assessment (GRA), Likert scales for bladder pain, urgency and frequency, and validated O'Leary-Sant IC symptom and problem indices. RESULTS: Significantly more patients treated with PSD597 rated their overall bladder symptoms as moderately or markedly improved on the GRA scale 3 days after completing the 5-day course of treatment (30% and 9.6%, respectively, for patients treated with PSD597 and placebo; P = 0.012). The treatment effects were also maintained beyond the end of treatment and are further supported by the secondary endpoints, including symptom and problem indices. The peak serum lidocaine concentration during the study was <2 microg/mL, and well below the toxic level (>5 microg/mL). CONCLUSION: This preliminary study showed that PSD597 was effective for providing sustained amelioration of symptoms of IC/PBlS beyond the acute treatment phase. The drug was safe, well tolerated and devoid of the systemic side-effects often experienced with oral drug administration. Long-term studies are needed to determine the optimum regimen to maintain this favourable treatment effect. PMID: 19021619 [PubMed - as supplied by publisher.
Theoharides TC, Kempuraj D, Vakali S, Sant GR. Department of Pharmacology and Experimental Therapeutics, Tufts University School of Medicine and Tufts Medical Center, Boston, Massachusetts, USA. OBJECTIVES: Interstitial cystitis/Painful bladder syndrome (IC/PBS) is a chronic bladder condition of unknown etiology and pathogenesis. However, there is evidence of bladder surface mucosal and glycosaminoglycans (GAG) dysfunction in IC/PBS and GAG replacement therapy has been used to treat the condition. The results of an open label, uncontrolled study of a dietary supplement designed to improve GAG mucopolysaccharides integrity (glucosamine sulfate, sodium hyaluronate and chondroitin sulfate) and reduce bladder wall inflammation (quercetin, rutin) are presented herein METHODS: Two hundred fifty two IC/PBS patients (25 men, 227 women; 18-69 years old), who had failed other treatments, took four CystoProtek capsules /day (mg/capsule: glucosamine sulfate, 120; chondroitin sulfate, 150; hyaluronate sodium, 10; quercetin, 150; rutin, 20). Symptoms were evaluated using a visual analogue scale (VAS) (severity range from 1-10) before and after treatment (< 6, 6-12 or > 12 months). The women were divided into two severity groups - a more severe A group with a baseline mean VAS score greater than or equal to 5 and a less severe B group with a mean score < 5. RESULTS: Male patients (55.72 +/- 9.53 years, n = 25) had a mean VAS score at baseline of 7.6 +/- 1.63 which fell 51.8% to 3.94 +/- 2.46 (p < 0.0001) after 12.46 +/- 8.76 months of treatment. The women (n = 227) experienced a 48.8% reduction in the mean VAS score (p < 0.0001) after 11.2 +/- 8.7 months. The mean VAS score in Group A (49.72 +/- 11.39 years, n = 207) fell 52.1% from 7.91 +/- 1.55 to 3.79 +/- 2.37 (p < 0.0001) after 11.06 +/- 8.18 months and in Group B (52.40 +/- 10.19 years, n = 20) fell 43.5% from 3.15 +/- 0.92 to 1.78 +/- 1.63 (p = 0.013) after 10.10 +/- 5.80 months. Patients in Group A and B were further subdivided into Groups A1, B1 (> 12 months), A2, B2 (6-12 months) and A3, B3 (< 6 months treatment); improvement was statistically significant in all the more severe Group A treatment duration subgroups. CONCLUSIONS: Dietary supplements targeting the bladder GAGs (chondroitin, glucosamine, hyaluronate) and bladder inflammation (quercetin, rutin) are useful in the treatment of refractory IC/PBS. Prospective randomized trials of such supplements are warranted in both treatment refractory and treatment naïve patients. Finns mer att läsa om detta naturmedel på http://www.cysto-protek.com PMID: 19046494 [PubMed - in process]
Bladder necrosis following hydrodistention in patients with interstitial cystitis Zabihi N, Allee T, Maher MG, et al. J Urol 2007;177:149-52 Geffen School of Medicine at University of California-Los Angeles, Los Angeles, USA. PURPOSE: Bladder hydrodistention is used to diagnose and treat patients with interstitial cystitis. This procedure has been shown to have minimal morbidity and provide symptomatic relief in a subset of patients with interstitial cystitis. We report our experience with almost total bladder necrosis after hydrodistention at 2 institutions. To our knowledge this rare complication has not been previously reported in the literature. We also reviewed the literature regarding complications of hydrodistention and discuss their possible etiology. MATERIALS AND METHODS: We report 3 cases of bladder necrosis after therapeutic hydrodistention for interstitial cystitis at 2 institutions. All records were reviewed, and the clinical presentation, findings and treatments are discussed. A literature review was performed to evaluate the effectiveness and complications of hydrodistention for interstitial cystitis. RESULTS: There were 2 female and 1 male patient between ages 29 and 46. All patients had a previous diagnosis of interstitial cystitis and had been previously treated with hydrodistention. All patients presented with severe abdominal pain and had necrosis of the entire bladder wall with sparing of the trigone. Two patients were treated with supratrigonal cystectomy. A review of the literature revealed little data on the effectiveness of hydrodistention for interstitial cystitis. CONCLUSIONS: Vesical necrosis is a rare but devastating complication of hydrodistention. It can occur in young patients in the absence of a contracted bladder and it usually presents as severe postoperative abdominal pain. At exploration bladder necrosis with sparing of the trigone was observed. All patients required enterocystoplasty.
Many inflammatory and neuropathic pain states are resistant to current therapies. It has recently been shown that in many of these disease states there is a large increase in levels of a protein called Nerve Growth Factor (NGF). This protein exacerbates painful responses by sensitising sensory neurons or by activating inflammatory cells. NGF acts via a receptor, called tyrosine kinase (TrkA), present on the surface of sensory neurons. The Dawbarn/Allen group has identified the region on the TrkA receptor that binds to NGF. They have produced this small part of the protein (called TrkAD5) in bacteria and purified it to homogeneity, and have determined its structure by X-ray crystallography (Figure 1), in collaboration with Leo Brady in the Department of Biochemistry. In situations where there is inflammatory pain, injection of TrkAD5 binds to excess NGF, rendering it inactive and thereby alleviating the pain. In addition, aspects of asthma relating to sensitisation of sensory neurons are currently untreatable. In a collaboration with Christine Nassenstein and Armin Braun, at the University of Hanover, the group have shown that TrkAD5 controls this aspect of asthma. Thus TrkAD5 is unique in that it is the only compound which has been able to do this. This binding domain is covered by four University patents. The protein, renamed as REN1820, has been out-licensed to a pharmaceutical company for clinical application. In collaboration with a number of groups worldwide the Dawbarn/Allen group have shown that this protein is effective in models of interstitial cystitis, pancreatitis, inflammatory pain, neuropathic pain and asthma. The protein is now at the stage of technology transfer for large-scale production to GMP (good manufacturing practice). It is envisaged that REN1820 will initially be used for the treatment of interstitial cystitis by subcutaneous injection. Se: http://www.bris.ac.uk/researchreview/2005/11321608504
The effects of Foods, Beverages and Supplements on the Symtoms of interstitial cystitis Barbara Shorter, Leslie Kushner, Robert M. Moldwin, CW Post Campus, Long Island University, Brookville, NY, Long Island Jewish Medical Center, New Hyde Park, NY. Introduction and Objective The etiology of interstitial cystitis (IC), a debilitating, multifactorial syndrome of the bladder, eludes doctors. Various causes have been speculated. consequently IC is a complex condition to treat. Among the non-traditional approaches used for IC, dietary changes seem to improve symptoms in some individuals. Most of the data gathered on diet as it affects IC symptoms is anecdotal. We developed a questionnaire in order to determine if certain foods, beverages and/or dietary supplements are perceived as increasing or decreasing symptoms of IC. Methods A questionnaire designed to detect whether food, beverages and/or supplements have an effect on bladder symptoms was developed and administered to patients meeting NIDDK criteria for IC (n=37). In addition to answering general questions about the effect of comestibles on IC symptoms, subjects were asked to indicate whether each of over 150 individual items worsens symptoms, slightly worsens symptoms, has no effect, slightly improves symptoms, improves symptoms, or the item is not eaten by the subject; responses were recorded as –2, -1, 0, +1, +2, de, respectively, and a mean value for each item was generated. Results Nearly three quarters (73%) of the IC patients surveyed indicated that consumption of certain foods or beverages caused exacerbation of symptoms; 5% indicated that foods or beverages did not exacerbate symptoms and 22% didn’t know. 18% of the subjects indicated that consumption of certain foods or beverages reduced symptoms of IC. Greater than 75% of subjects reported exacerbation of IC symptoms after ingestion of coffee, cola, grapefruit and vinegar; 50-75% reported exacerbation of IC symptoms after ingestion of spicy foods, pizza, alcoholic beverages, strawberries, tomatoes. Subjects tended to avoid the most bothersome foods, indicating that they did not eat chili (50%), orange juice (41%), lemons (41%), spicy foods (41%), pineapple (36%), decaffeinated coffee (36%), grapefruit (32%), alcoholic beverages (32%), coffee (27%), oranges (27%), cola (27%), vinegar (27%). The rank order of specific comestibles which exacerbated symptoms are coffee, grapefruit, cola, vinegar, alcoholic beverages>tomatoes, tomato products>lemons, orange juice, chili> strawberries, pineapple, oranges, onions, pizza>chocolate>decaffeinated coffee, apples; coffee ranked as the most bothersome with a mean value of –1.85. Conclusions There is a large cohort of IC patients whose symptoms are exacerbated by ingestion of specific comestibles. The most frequently reported and the most bothersome comestibles include items containing caffeine, citrus fruits and juices, tomatoes and tomato products, items containing vinegar and alcoholic beverages.
Horseback Riding: Impact on Sexual Dysfunction and Lower Urinary Tract Symptoms in Men and Women Alanee S, Heiner J, Liu N, Monga M. Department of Urologic Surgery, University of Minnesota, Minneapolis, Minnesota. OBJECTIVES: To determine whether subjects engaged in horseback riding are more likely to be affected by sexual dysfunction and lower urinary tract symptoms than those engaged in sports with less perineal impact. MATERIAL AND METHODS: Surveys evaluating the presence of and the risk factors for sexual dysfunction and urinary symptoms were distributed among members of equestrian clubs, swimming clubs, and individual horseback riders and swimmers. About 327 surveys were distributed by hand at horse shows and swimming pools. A total of 2000 surveys were sent by direct mail to random members of 1 national equestrian organization and 1 national swimming organization. We also evaluated bicycle habits as a possible confounding factor. RESULTS: There was no significant association between horseback riding and lower urinary tract symptoms (P = .1759) and sexual dysfunction (P = .1793) in males. The same applies to the association of horseback riding and lower urinary tract symptoms (P = .5036) and sexual dysfunction (P > .05) in females, although there was a trend toward a protective association between horseback riding and stress incontinence (P = .0567). Years of bicycling (P = .04) and hardness of the bicycle seat (P = .02) were associated with an increased prevalence for lower urinary tract symptoms in women. CONCLUSIONS: Regular participation in horseback riding is not significantly associated with increased prevalence of lower urinary tract symptoms or sexual dysfunction, although it may be associated with decreased prevalence of stress urinary incontinence. Bicycle riding may be associated with higher prevalence of lower urinary tract symptoms in women. PMID: 18950839 [PubMed - as supplied by publisher]
NOFUS är en norsk organisation för urologiska sjukdomar. Från deras septembernummer 2000 har vi saxat följande: Interstitiell Cystitt - en sykdom uten klare svar. Tage Hald, professer, dr.med., Danmark. Årsaker
Diese to teorierna er ikke helt uforenlige, da en slimhinnedefekt kan vare årsaken til en immunreaksjon eller omvendt. Behandling Professor Hald nämner också i artikeln, att för svårt drabbade måste man tillämpa andra lösningar i form av olika kirurgiska ingrepp.
Från AUA/American Urology Association meeting 2005 Jane Meijlink, International Interstitial Cystitis Patient Network Foundation har gjort en utmärkt sammanställning beträffande IC på URL http://www.iicpn-foundation.org/NewsReviewsReportAUA2005SanAntonio.htm
Smärtlindring vid IC, från AUA meeting 2005 Dr. Christopher Payne, Stanford University, USA. When Dr. Payne took the podium, he urged his colleagues to treat IC patients’ chronic pain - something many urologists are reluctant to do and aren’t comfortable with. "Pain management is, in and of itself, an appropriate and realistic goal, and it’s appropriate for the urologist. It’s our natural role as physicians to relieve pain and suffering and we have the tools to do it. We can do this," he said. When pain is chronic, patients need much more than regular care, he emphasized. They need more evaluation, they need help from other specialists because other organ systems are often affected, and they need to work with a primary care physician who will coordinate their care over the long term. Because we can’t cure the problem, the goal has to be to improve function. "we can link our use of pain medication and higher doses of pain medication to higher functional improvement and better quality of life. That is what’s realistic. That’s what we can accomplish," Dr. Payne told his colleagues. Pain is complex, including more typical pain, deep organ pain, and nerve pain, so no single medication can take care of it all. Treatment has to be multimodal, he said, including different types of medications (opioids, nonsteroidal anti-inflammatory drugs, antidepressants, anticonvulsants, membrane stabilizers, and others), procedures such as nerve and epidural blocks, psychological support, and physical therapy. Combining medications can not only give better pain relief but can also reduce side effects. But opioids, he said, are the mainstay of therapy. They’re well accepted for cancer pain, for AIDS pain, for neuropathic pain, and for many other disorders, "and yet for IC, he pointed out, "opioids are frequently not considered, and when they’re considered, they’re not offered. I believe this is not appropriate." Dr. Payne tried to dispel misconceptions that many have about opioids. Tolerance and dependence, which are to be expected, are not addiction. Very often, patients who take opioids need higher doses over time to achieve the same relief, which is tolerance, and urologists should expect that. Dependence is a physiological response to stopping opioid medication that is nearly universal and it is not addiction, he emphasized. "Addiction is totally different. It is a psychologic and behavioral problem in which a person uses a drug compulsively despite evidence that it’s harming them and continuing to use it despite the harm. The person exhibits the behavior we associate with addicts to procure medication. This is a rare problem in patients who are being treated for a medical disease and chronic pain if they’ve been properly evaluated and followed." He advised his colleagues to use opioid contracts to protect themselves and patients from potential problems, and informed the audience that model contracts are available on the internet and from pain specialists. Dr. Payne recommended using immediate-release preparations only for finding out what doses of long-acting opioids patients need or for patients who don’t need pain medication every day and can manage with low doses. They can also be used for breakthrough pain as doctors find the right dose of longer-acting medication. There are a number of extended-release medications, and he encouraged urologists treating IC patients "to pick at least one and become familiar with how to use that agent." Dr. Payne uses methadone primarily but also uses long-acting morphine preparations. Other choices include long- acting oxycodone (Oxycontin), fentanyl (Duragesic), and hydromorphone (Palladone). Meperidine, propoxyphene, and mixed agonist-antagonists are poor choices, he said. With opioids, he added, "it’s very important to anticipate and treat the side effects, particularly constipation. You always start with stool softeners with the original prescription. We warn the patient about the potential need for laxatives, and we don’t want to see somnolence (drowsiness). That’s a bad side effect. Remember, we’re trying to improve function. So if we see somnolence, and somebody can’t focus at work, we know we’ve gone too far." Dr. Payne left his colleagues with these thoughts: "I believe that it’s appropriate to treat chronic pain, even when the underlying disease is not known or is untreatable. Multimodality therapy is the most effective way to treat chronic pain. Opioids are the keystone of treating chronic pain in most patients. And we need to focus our treatment on improving activity, on improving goals, improving function and quality of life, not aiming at total relief of pain. And I think, if we can do that, we’ll make a great impact on our patients." Ovanstående finns även för utskrift i pdf-format på en A4-sida.
Risk Factors For Opiate Medication Abuse In Chronic Pain Patients Identified From: The Journal of Pain 2005 September; 6:620-629 BERKELEY, CA (UroToday.com) - Painful bladder syndrome / interstitial cystitis can be considered a chronic pain syndrome. As with other chronic pain syndromes, a great many patients are left with continued pain even after repeated treatment attempts. For these patients, long-term use of opiate medications may represent the best and most cost-effective medical treatment available. Chronic pain is increasingly recognized as a significant contributor to patient suffering and disability, provider frustration, and increased health care costs. Schieffer and colleagues assessed the influence of medication beliefs, symptom severity, disability, mood, and psychiatric history on opiate medication misuse behaviors in 288 chronic pain patients using questionnaires and electronic medical records. Consistent with previous findings, the data indicated that a history of substance abuse is related to higher rates of medication misuse behaviors, despite similar dosages and self-rated opiate effectiveness. Misusers believed more strongly in the potential for opiate addiction and that they required higher doses than others, but also had greater belief in opiate effectiveness and the importance of free access. Although both anxiety and substance abuse history are related to medication misuse, multivariate analysis indicated that these factors can be seen as mediated by medication beliefs. This paper highlights the complexity of using chronic narcotics for the relief of nonmalignant pain. Self-attributions regarding opiate treatment interact with anxiety to produce a high rate of opiate misuse in some populations. The institution of opiate therapy for painful bladder syndrome is not to be undertaken lightly, and expert consultation with a pain specialist would seem to be prudent before imparting on this treatment pathway.
Diurnal cortisol variations and symptoms in patients with Interstitial Cystitis, Tyskland J Urol 2002 March;167(3):1338-1343 Susan K. Lutgendorf, Karl J. Kreider, Nan E. Rothrock, Anna Hoffman, Clemens Kirschbaum, Esther M. Sternberg, M. Bridget Zimmerman, Timothy L. Ratliff. From the Departments of Psychology, Urology, Biostatistics (School of Public Health) and Microbiology, and Interdisciplinary Graduate Program in Immunology, University of Iowa, Iowa City, Iowa, Institute of Physiological Psychology II, University of Dusseldorf, Dusseldorf, Germany, and National Institute of Mental Health, Bethesda, Maryland. Purpose: Little attention has focused on systemic factors that may allow a state of chronic bladder inflammation to be established and maintained in interstitial cystitis cases. Abnormalities of the hypothalamic-pituitary-adrenal feedback system result in poorer regulation of the inflammatory response and are present in many chronic inflammatory and pain conditions, of which some have high co-morbidity with interstitial cystitis. Materials and Methods: A total of 48 patients with interstitial cystitis and 35 healthy, age matched controls collected 24-hour urine samples and 3 days of salivary samples at 7 to 8 a.m., 4 to 5 p.m. and 8 to 9 p.m. for cortisol analysis. In addition, they completed a concurrent symptom questionnaire. Prospective symptom diaries also were completed in the month before sampling. Results: Mean urinary or salivary cortisol did not differ in patients and controls. However, patients with interstitial cystitis and higher morning cortisol had significantly less pain and urgency, while those with higher urinary free cortisol reported less overall symptomatology (p <0.05). Relationships with morning cortisol were also observed when controlling for co-morbid conditions known to be affected by the hypothalamic-pituitary-adrenal axis, such as fibromyalgia, chronic fatigue and rheumatoid arthritis. Patients with morning cortisol less than 12.5 nmol./l. were 12.8 times more likely to report high urinary urgency than those with values above this cutoff. Conclusions: These findings imply that regulation of the hypothalamic-pituitary-adrenal axis may be associated with interstitial cystitis symptomatology and there may be different diurnal hypothalamic-pituitary-adrenal patterns in patients with interstitial cystitis who do and do not have co-morbid conditions. These findings may have treatment implications for patients with interstitial cystitis who have early morning cortisol deficiencies.
A Comparison of Multiple Urine Markers for Interstitial Cystitis THE JOURNAL OF UROLOGY June 2002;167:2461-2469 DEBORAH R. ERICKSON; SHARON X. XIE; VEER P. BHAVANANDAN; MARCIA A. WHEELER; ROBERT E. HURST; LAWRENCE M. DEMERS; LESLIE KUSHNER; SUSAN K. KEAY* From the Division of Urology and Departments of Health Evaluation Sciences, Biochemistry and Medicine and Pathology, Pennsylvania State University, College of Medicine, Hershey, Pennsylvania, Section of Urology, Yale School of Medicine, New Haven, Connecticut, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, Department of Urology, Long Island Jewish Medical Center, New Hyde Park, New York, and Division of Infectious Diseases, University of Maryland School of Medicine, Baltimore, Maryland Purpose: We measured several urine markers in 24-hour specimens from patients with interstitial cystitis and healthy controls. For each marker we determined whether the urine level was significantly different in interstitial cystitis and control cases, and whether the marker level correlated with the symptom score. Materials and Methods: Study participants included 36 female patients with interstitial cystitis and 36 age matched female volunteers. Multiple urine aliquots were obtained to measure the various markers. Results: Certain markers were significantly increased in interstitial cystitis, including anti-proliferative factor, epidermal growth factor, insulin-like growth factor (IGF) binding protein-3 and interleukin (IL)-6. Markers significantly decreased in interstitial cystitis were heparin-binding epidermal growth factor-like growth factor, cyclic guanosine monophosphate and methylhistamine. Other markers were not significantly different in the interstitial cystitis and control groups, including total glycosaminoglycans, epitectin, hyaluronic acid, IL-8, IL-1 and nitrates plus nitrites. IGF-1 was undetectable in 24-hour urine samples but spot voided samples from the same interstitial cystitis population had IGF-1 levels similar to previously reported levels. The only significant association of marker with symptom score was a positive correlation of IL-6 with nocturia. For all markers the conclusions were the same whether the marker was normalized to creatinine or to 24 hours. Conclusions: This study confirmed several previously reported urine alterations in interstitial cystitis, including increased anti-proliferative factor, epidermal growth factor, IGF binding protein-3 and IL-6, and decreased heparin-binding epidermal growth factor-like growth factor and cyclic guanosine monophosphate. Of all markers studied anti-proliferative factor had the least overlap in the interstitial cystitis and control groups, and so it is the most likely candidate to become a diagnostic test.
Ashok Batra, MD, State University of New York Health Science Center, Syracusa. Infect Urol 12(6):155-158, 1999. Vi bedömer den här artikeln som mycket intressant och vi har därför tagit med denna artikel i sin helhet. Du når den på en undersida genom att klicka på Interstitial Cystitis Update. Artikeln innehåller även NIADDK Research Definition of Interstitial Cystitis.
J Urol 2002 Jun;167(6):2470-2472 Peeker R, Fall M. Department of Urology, Sahlgrenska University Hospital Goteborg, Goteborg, Sweden. PURPOSE: Interstitial cystitis is a bothersome condition in urological practice. There is continuous discussion on the extent and demarcation of this syndrome. Accumulated evidence indicates that interstitial cystitis is a heterogeneous syndrome. Today it is often divided into classic and nonulcer disease. Compared with classic interstitial cystitis the nonulcer type appears different in terms of demographic, endoscopic and histological findings as well as in the response to various types of treatment. However, in clinical series subdivision is not always performed, which makes it difficult to draw conclusions. We determined whether there are additional dissimilarities in clinical presentation in the 2 subtypes of interstitial cystitis. MATERIALS AND METHODS: We evaluated 130 patients with classic and 101 with nonulcer interstitial cystitis diagnosed according to National Institute for Diabetes and Digestive and Kidney Diseases criteria by surveying the clinical records, including voiding diaries. RESULTS: Patients with nonulcer disease were younger at diagnosis (p <0.0001) and at symptom onset. Furthermore, there was a marked and significant difference in bladder capacity while patients were under general anesthesia (p <0.0001). CONCLUSIONS: The current findings together with previous findings clearly demonstrate that the 2 subtypes of interstitial cystitis represent separate entities. We suggest refining the National Institutes of Health-National Institute for Diabetes and Digestive and Kidney Diseases criteria, so that subtyping scientific materials is considered mandatory, hence, ensuring that the 2 subtypes are evaluated separately in clinical studies. PMID: 11992059
A diagnostic in vitro urine assay for Interstitial Cystitis, USA En artikel på engelska av urologerna S. Key, C-O Zhang, M.K Hise m.fl. Behandlar forskning om diagnos rörande Interstitiell Cystit. Klicka här för att läsa artikeln. Filen är på cirka 149 kB och i pdf-format (avsedd för Adobe Acrobat).
Chlamydia pneumoniae Implicated in Pathogenesis of Interstitial Cystitis, (Reuters Health) WESTPORT, CT (Reuters Health) Jun 04, 2001. Researchers from Vanderbilt University, in Nashville, Tennessee, have evidence of a potential link between Chlamydia pneumoniae and interstitial cystitis. In a presentation at the American Urological Association meeting in Anaheim, California, Dr. Jenny J. Franke reported that 14 of 17, or 82%, of patients with biopsy-confirmed interstitial cystitis had tissue cultures positive for C. pneumoniae. In contrast, only 1 of 6, or 16%, of control patients without interstitial cystitis were positive for C. pneumoniae. "Our institution has investigated the association of C. pneumoniae and interstitial cystitis using two separate techniques. Previously we used polymerase chain reaction (PCR) and our current study used cell culture. Both techniques have shown a statistically significant correlation between interstitial cystitis and urinary C. pneumoniae infection," Dr. Franke said in an interview with Reuters Health. This implies that C. pneumoniae may be involved in the pathogenesis of interstitial cystitis in certain patients, the researcher said. "A patient's genetic susceptibility and C. pneumoniae strain virulence may play important roles and require further investigation." She cautioned that the findings need to be validated by similar studies at other institutions, with evaluations performed following response to appropriate antimicrobial therapy.
THE JOURNAL OF UROLOGY 2000;163:1112-1115 Ralph Peeker, Frank Aldenborg, Annica Dahström, Sonny L. Johansson Jia-Yi Li, Magnus Fall. From the Urology Division, Department of Surgery, and Department of Pathology, Sahlgrenska University Hospital, and Department of Neurobiology, Göteborg University, Göteborg, Sweden, and Department of Pathology and Microbiology, and Eppley Institute for Research on Cancer and Allied Diseases, University of Nebraska Medical Center, Omaha, Nebraska Abstract: Purpose: Interstitial cystitis is a chronic debilitating condition which mainly affects women. Accumulated evidence indicates that interstitial cystitis is a heterogeneous syndrome. The nonulcer subtype appears different than classic interstitial cystitis in regard to symptoms, and endoscopic and histological findings as well as response to various treatments. We further explore the neurogenic nature of this disease using indirect immunofluorescence to evaluate the presence and density of various autonomic and sensory nerve fibers. Materials and Methods: Specimens from the bladder wall of 6 patients with classic interstitial cystitis, 7 with nonulcer interstitial cystitis and 6 controls were evaluated to determine the presence and density of nerve fibers containing tyrosine hydroxylase, calcitonin gene-related peptide, neuropeptide Y and substance P using specific antibodies, and the general presence of nerve fibers using a mixture of antibodies against nerve filament, neuron specific enolase and S-100 protein. Results: Increased density and number of nerve fibers immunoreactive for tyrosine hydroxylase were noted in interstitial cystitis cases compared to controls. Furthermore, there was a difference between classic and nonulcer disease in the overall density of nerves using the antibody mixture. Conclusions: Our findings indicate an altered peripheral sympathetic innervation in interstitial cystitis cases, which may be an indication of primary neurogenic etiology. The difference in nerve density observed after incubation with the antibody mixture between classic and nonulcer interstitial cystitis supports the hypothesis that the 2 forms represent separate entities.
Cimetidine in painful bladder syndrome: A histopathological study BJU Int 2001 Aug;88(3):183-6 Dasgupta P, Sharma SD, Womack C, Blackford HN, Dennis P. Department of Urology, Peterborough Hospitals NHS Trust, Edith Cavell Hospital, Peterborough, UK. prokarurol@cs.com OBJECTIVE: To determine whether oral cimetidine, which reportedly improves symptoms in 60-70% of patients with painful bladder syndrome/interstitial cystitis has a similar mechanism of action on the human bladder and involving a similar peptidergic pathway as it has in human stomach, where it alters histamine-gastrin reactions mediated via H2 receptors and a proton pump. PATIENTS AND METHODS: Fourteen patients (13 women and one man, mean age 51 years) with refractory bladder pain and irritative urinary symptoms were treated with cimetidine. The response to cimetidine was assessed by outpatient follow-up and an analogue pain score. Bladder biopsies from eight patients were stained with haematoxylin and eosin, and a polyclonal antibody to gastrin, with counterstaining using toluidine blue, to detect mast cell granules containing histamine. Biopsies from normal areas of the bladder from an age-matched control group of patients with transitional cell carcinoma of the bladder were stained similarly. Human stomach and colon were used as positive controls for gastrin and toluidine blue, respectively. The clinical response to cimetidine was compared with the histology in a blinded fashion. RESULTS: Eight of the patients responded well to cimetidine; none of the biopsies showed evidence of carcinoma in situ. Although G cells in the stomach stained well for gastrin none of the bladder biopsies showed gastrin-like immunoreactivity, apart from some nonspecific urothelial staining. Numerous mast cells with crimson granules and pale nuclei were visible in three patients and fewer in three others; their presence or absence did not correlate with the symptomatic response. CONCLUSIONS: Cimetidine is a useful medical treatment for bladder pain but the presence or absence of gastrin or histamine-like immunoreactivity does not explain its therapeutic benefit.
J. Urol 1998 May; 1 59(5):1483-6; discussion 1486-7 Peters KM, Diokno AC, Steinert BW, Gonzalez JA Department of Urology, William Beaumont Hospital, Royal Oak, Michigan, USA. PURPOSE: Interstitial cystitis is a severe debilitating bladder disease characterized by unrelenting pelvic pain and urinary frequency. A prospective, double-blind, placebo controlled study of the use of intravesical bacillus Calmette-Guerin (BCG) in the treatment of interstitial cystitis was recently completed with a mean followup of 8months. Results demonstrated a 60% BCG response rate, compared to a 27% placebo response rate. We now report the long-term followup results of those patients who received intravesical BCG. MATERIALS AND METHODS: Subjects randomized to receive BCG were followed at routine intervals with questionnaires and voiding diaries identical to those in the blinded study. Adverse events were closely monitored in the treatment and followup phases of the study. Subject baseline values were compared to followup data. RESULTS: Of the BCG responders mean followup was 27 months (range 24 to 33), and 8 of 9 (89%) continue to have an excellent response in all parameters measured. The global interstitial cystitis survey improved 70%, daily voids decreased 3 1 %, nocturia improved 54%, mean voided volume increased 6 1 %, pelvic pain decreased 8 1 %, vaginal pain decreased 7 1 %, urgency decreased 7 1 % and dysuria decreased 82%. Overall well-being improved 54% and the Rand-36 quality of life survey overall improved 64%. In 86% of the patients (6 of 7) dyspareunia resolved. Of the initial BCG nonresponders there was no significant difference in interstitial cystitis symptomatology from baseline to last followup, suggesting that BCG does not worsen interstitial cystitis symptoms. No long-term adverse events from BCG were noted. CONCLUSIONS: Intravesical Tice BCG is safe, effective and durable in the treatment of interstitial cystitis. Of those patients who received only 6 weekly treatments and responded favorably 89% continue to have an excellent response with followup ranging from 24 to 33 months. Comment in: J Urol 1998 Dec- 160(6 Pt 1):2163 PMID: 9554338, Ul: 98213000
Ueda T, Tamaki M, Ogawa O, Yamauchi T, Yoshimura N Department of Urology, Kouga Public Hospital, Shiga, Faculty of Medicine, Kyoto
University, Kyoto and Kitano Hospital, Osaka, Japan, and Department of
Pharmacology, University of Pittsburgh School of Medicine, Pittsburgh,
Pennsylvania. PURPOSE: We examined the efficacy of Suplatast Tosilatedouble dagger (IPD-1151T), a new immunoregulator that suppresses helper T cell mediated allergic responses, including IgE production and eosinophilic inflammation for treating patients with interstitial cystitis. MATERIALS AND METHODS: A total of 14 women (average age 43.7 years) with interstitial cystitis, which was nonulcerative in 13 and ulcerative in 1, were treated with 300 mg. IPD-1151T orally daily for 12 months. All patients received laboratory assessments, including hematology (eosinophils and CD20 positive cells) and serum chemistry (IgE, and interleukin-4 (IL-4) and 5, and immunohistochemical analyses of urine leukocytes (CD45RO positive cells as a T cell marker) before treatment. These parameters were also measured 4 and 12 months after continuous treatment. The voiding chart, and interstitial cystitis symptom and problem indexes were evaluated before and after IPD-1151T treatment. RESULTS: IPD-1151 Treatment for 1 year resulted in a significantly increased bladder capacity and decreased symptoms, such as urinary urgency, frequency and lower abdominal pain, in patients with nonulcerative interstitial cystitis. These effects also correlated with a reduction in blood eosinophils, CD20 positive cells and IgE, and urine CD45RO positive memory T cells. No major side effects were observed. CONCLUSIONS: Our study suggests that immunological responses are involved in the development of interstitial cystitis symptoms. IPD-1151T could be a new oral agent for treatment of voiding symptoms and bladder pain in patients with interstitial cystitis. PMID: 11061880
Urol 2001 Nov;166(5):1734-7 Bouchelouche K, Nordling J, Hald T, Bouchelouche P. Department of Urology, Herlev Hospital, University of Copenhagen, Herlev and Department of Clinical Biochemistry, Koege Hospital, County of Roskilde, Denmark. PURPOSE: The presence of leukotriene D4 receptors in human detrusor myocytes and increased urinary leukotriene E4 in patients with interstitial cystitis and detrusor mastocytosis imply a role for cysteinyl containing leukotrienes as proinflammatory mediators in this disease. We examined the efficacy of the cysteinyl leukotriene 1 receptor antagonist montelukast for treating patients with interstitial cystitis and detrusor mastocytosis. MATERIALS AND METHODS: Ten women in whom interstitial cystitis was diagnosed according to National Institute of Diabetes and Digestive and Kidney iseases criteria and who also had detrusor mastocytosis with a minimum of 28 mast cells per mm.2 muscle tissue were included in this study. Patients received a single dose of montelukast daily for 3 months. The efficacy of treatment was determined by 24-hour urinary frequency, nocturia and pain using visual analog scales. RESULTS: After 1 month of montelukast treatment there was a statistically significant decrease in 24-hour urinary frequency, nocturia and pain which persisted during the 3 months of treatment. After 3 months 24-hour urinary frequency had decreased from 17.4 to 12 voidings (p = 0.009), nocturia had decreased from 4.5 to 2.8 (p = 0.019) and pain had decreased from 46.8 to 19.6 mm. on a visual analog scale (p = 0.006). No side effects were observed during treatment. CONCLUSIONS: Montelukast treatment resulted in significant improvement in urinary frequency and pain. Its efficacy for decreasing urinary frequency and pain imply a role of leukotriene receptor antagonists for managing interstitial cystitis but further placebo controlled clinical studies are needed. PMID: 11586212 [PubMed - in process]
Volume 2, Issue 4 , December 2004, Pages 179-186 Neurourology Jørgen Nordling Department of Urology, Herlev Hospital, University of Copenhagen, Herlev Ringvej 75, DK2730 Herlev, Denmark. Interstitial cystitis is a chronic disease characterized by bladder pain, frequency and urgency. Because of lack of definition and specific diagnostic criteria terminology today changes towards Painful Bladder Syndrome (PBS) reserving the diagnosis Interstitial Cystitis (IC) for a disease with typical cystoscopic and histological features yet to be defined. Diagnosis and evaluation: Patients with bladder pain, frequency and urgency must have other pathologies like bacterial, radiation or chemical cystitis, pelvic tumors, infravesical obstruction or urethral diverticula excluded by examination of the urine, endoscopy or other relevant investigations. Evaluation by cystoscopy in general anaesthesia with bladder distension and bladder biopsy gives information on presence of Hunner's ulcer, glomerulations, bladder capacity and bladder wall inflammation, which have influence on treatment strategy and prognosis. Treatment: An abundance of treatments have been suggested, but very few have been subjected to proper controlled trials. Patient counseling and instructions in self care and dietary initiatives are important. Physical therapy for primary or secondary myofascial tensions in the pelvis might be helpful. Oral treatment with antihistamines and pentosanpolysulphate is well established, while leucotriene receptor antagonists, cyclosporine and many others are still investigational. Bladder irrigation with DMSO, hyaloronic acid and heparin is widely used, while BCG, lidocain, capsaicin and RTX have been reported. Pain treatment spans from mild analgesics over tricyclic antidepressants (amitryptylin) and antiepileptics (gabapentin) to opioids. Surgical intervention includes bladder distension, resection of Hunner's ulcer, bladder augmentation, urinary diversion and cystectomy depending on disease severity and symptomatology.
Long-term outcome of patients with Interstitiell cystitis treated with low dose Cyclosporine A. Journal of Urology June 2004. Sairanen J, Forsell T, Ruutu M. Department of Urology, Helsinki University Hospital, Helsinki (JS, MR), Department of Surgery, Kymenlaakso Central Hospital, Kotka (TF), and Department of Surgery, Paijat-Hame Central Hospital, Lahti (JS), Finland. PURPOSE: We evaluated patients with interstitial cystitis who had been on Cyclosporine A (i Sverige Ciklosporin med handelsnamnet Sandimmun) treatment for at least a year. Symptom improvement on micturition charts and subjective expression of bladder pain were recorded. Side effects and safety of medication were evaluated. MATERIALS AND METHODS: A total of 23 patients (20 females and 3 males) fulfilling National Institute for Diabetes and Digestive and Kidney Diseases criteria of interstitial cystitis were included in this study. Age of patients at followup was 65.7 +/- 7.6 years (mean +/- SD). Mean followup was 60.8 +/- 35.7 months. Before starting Cyclosporine A treatment multiple first line therapies had been tried without clinical help. RESULTS: The number of voidings in 24 hours was 20.8 +/- 6.3 before treatment. After a year of Cyclosporine A treatment it was decreased to 10.2 +/- 3.8 (p < 0.001). Maximal bladder capacity increased from 161.8 +/- 74.6 to 360.7 +/- 99.3 ml in a year (p < 0.001). Mean voided volume increased from 101.4 +/- 42.7 to 246.4 +/- 97.9 ml (p < 0.001). The effect was maintained throughout followup. Of 23 total patients 20 reported no bladder pain on Cyclosporine A treatment and 11 patients stopped treatment due to a good clinical effect. In 9 patients symptoms recurred within months but disappeared again after Cyclosporine A treatment was restarted. Side effects of medication were infrequent. CONCLUSIONS: Cyclosporine A treatment was safe and effective in treating interstitial cystitis. The achieved therapeutic effect was maintained in the long term. Cessation of medication led to recurrence of symptoms in most cases. PMID: 15126772
• Intertitial Cystitis update: http://www.urotoday.com/images/conferences/MIR_2008/mir_2008_interstitial_cystitis.pdf
Kvinnans könsorgan
|