|
Statistik (prostatit, IC) och historik
— sjukdomarna är betydligt vanligare än man tror —
Någon studie över hur många som är drabbade av kronisk prostatit/CPPS och interstitiell cystit/IC har tyvärr inte gjorts i Sverige. De resultat som redovisats i olika sammanhang för Sverige beträffande incidens och prevalens, bygger därför till stor del på jämförelser med studier från andra länder. Nedanstående studier beträffande behandlingsresultat (t.ex. NIH), ger en helt annan (negativare) bild av än vad som ofta redovisats av allmänpraktiserande läkare och urologer i Sverige. En av anledningarna till detta är troligtvis, att de flesta läkare har bristfälliga kunskaper om kronisk prostatit och interstitiell cystit och misstror vad patienterna anser om sina besvär p.g.a. sjukdomen.
Typisk patient vid Prostatitis Center in Tucson, Arizona, USA The typical or average patient who comes to the Prostatitis Center in Tucson, Arizona for treatment of chronic prostatitis is about 38 years old (range 19 to over 70) and had symptoms for 8 years (range a few months to over 40 years). The average patient had seen many previous physicians, including several different urologists and had taken about 5 different antibiotics (maximum 13), several for multiple courses. The typical patient did have pelvic pain, but not all patients had appreciable pain as a symptom. Most patients reported that they had combinations of the following symptoms: 1. Pelvic pain 2. Urinary dysfunction 3. Sexual dysfunction. Almost all patients have more than one symptom. In about 2/3 of the patients, pain was the major symptom. In about 1/3 the patients, pain was not the major symptom. However, please note that for about 10 percent of the patients, their major symptom was not one of the three major symptoms listed above. None of the patients had a previous history of recurrent episodes of bacterial urinary tract infections, and thus none had a history of infections caused by the same organism, usually E coli, another Gram-negative organism, or enterococcus. Here in Tucson, almost none of the patients had any laboratory finding suggestive of a urinary tract infection - - - urinalysis or urine culture of a mid-stream urine (when the patient was not taking antibiotics). Regarding the expressed prostatic secretions (EPS) obtained from the first prostate massage, most patients had only a few white blood cells (WBCs) - - - polymorphonuclear cells (PMNs). However, and most importantly, the great majority of patients had numerous WBCs found in the EPS obtained on subsequent days by subsequent prostate massages. We could not help but notice that the information obtained from the first prostatic massage was misleading. In addition, our pathologists have found prostate inflammatory aggregates (PIAs) and Vega Bodies (PAS positive granules) in the EPS from the great majority of patients. As with WBCs, these other two pathologic findings are often not found in the EPS obtained from the first prostatic massage - - - often multiple massages, on separate days, are required. Please note that we believe that these two pathologic findings are diagnostic for prostatitis. Finally, we have isolated bacteria from the EPS in the great majority of our patients. (Several of the bacteria which we isolated from the EPS of our patients are included in the list of bacterial isolates recently published by the Seattle group - - - bacteria isolated from prostate biopsies. However, we frequently found bacteria not included on the Seattle list; and, we rarely if ever isolated some of the bacteria included on the Seattle list.). URL till kliniken är: http://www.prostate-usa.com
UROLOGY 71: 79–84, 2008. © 2008 Elsevier Inc. Shaun W H Lee, Men Long Liong, Kah Hay Yuen, Wing Seng Leong, Phaik Yeong Cheah, Nurzalina, AK Khan, Penang, Malaysia; John N Krieger, Seattle, WA OBJECTIVES: To examine the prevalence, characteristics, and impact of sexual dysfunction in our primary care referral population. METHODS: Participants seeking treatment for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) were recruited from general urology clinics. The subjects completed the National Institutes of Health-Chronic Prostatitis Symptom Index, International Index of Erectile Function-5, and selected questions from the University of Washington Symptom Score. Additional information on demographics and medical and treatment history were also obtained. Sexual dysfunction was defined as self-reported erectile dysfunction (ED) or ejaculatory difficulty, or both. RESULTS: Of 296 participants with CP/CPPS, 214 (72.3%) reported sexual dysfunction. The National Institutes of Health-Chronic Prostatitis Symptom Index total score averaged 22.5 _ 6.9 forparticipants with sexual dysfunction compared with 20.4 _ 7.8 for participants who did not report sexual dysfunction (P _ 0.03). Of the 214 participants with sexual dysfunction, 54 (25.0%) complained of ED only, 71 (33.4%) complained of ejaculatory difficulties only, and 89 (41.6%) complained of both ED and ejaculatory difficulties. Men reporting both ED and ejaculatory difficulty reported worse CP/CPPS symptoms (analysis of variance, P _ 0.042) and worse quality of life (analysis of variance, P _ 0.006) than men without sexual dysfunction. CONCLUSIONS: Sexual dysfunction was reported by almost three quarters of patients with CP/CPPS. Patients with CP/CPPS and sexual dysfunction experienced substantially worse symptoms, particularly worse quality of life, than other patients with CP/CPPS. Sexual dysfunction merits consideration as an important aspect of CP/CPPS and a potential outcome measure.
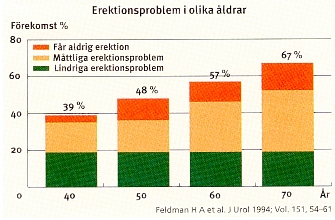
Svårigheter med erektion kan ha både fysiska och psykiska orsaker. Det kan vara olika prostatasjukdomar, diabetes, hjärt- och kärlsjukdomar och neurologiska sjukdomar. Även olika psykiska sjukdomar och hormonella faktorer kan ha inverkan på erektionen. Vissa mediciner kan också ge erektionsproblem. Stress, rökning och alkoholmissbruk ökar risken för erektionsproblem.
Erektionsproblem enligt broschyr från läkemedelsbolaget Lilly.
Allmänhetens kännedom om prostatit, USA. Most americans uninformed about prostate disease that affects one in two men, survey revals. A national survey shows that only 15 percent of Americans have heard of prostatitis, a sometimes serious and often painful condition that will affect more than half of the male population at some point in their lives. In response to these results, the survey sponsors (the American Foundation for Urologic Disease (AFUD), the Men's Health Network (MHN), and Bayer Corporation) are launching a national partnership to educate consumers about prostatitis. Consumers can call 800-206-6300 to obtain a free brochure about prostatitis, its symptoms, diagnostic tests, and available treatments. Enligt ISOPs bedömning är situationen med största sannolikhet densamma i Sverige?
Incidensen (hur många som drabbas) av prostatit i Sverige Från Läkartidningen sid. 3822, 2006-11-28 med rubriken: "Antibiotikabehandling vid kronisk prostatit saknar i princip evidens". Av de svenska läkarna Benny Holmström, överläkare, urologsektionen, kirurgkliniken, Gävle sjukhus och Pär Hallberg, med dr, ST-läkare, avdelningen för klinisk farmakologi, Akademiska sjukhuset, Uppsala. I artikeln skriver författarna bl.a.: "Prostatit förekommer hos 50 procent av alla män någon gång i livet." Se: http://www.lakartidningen.se/store/articlepdf/5/5561/LKT0648s3822_3828.pdf
Prevalensen (förekomsten) av prostatit i Sverige Professor Peter Wiklund, Urologkliniken vid Karolinska Sjukhuset skriver på sidan http://www.internetmedicin.se/dyn_main.asp?page=488&sub=108&item=4&main=ref. "Prostatit är den vanligaste urologiska orsaken till att män under 50 år uppsöker läkare. Nyare epidemiologiska studier visar att prevalensen (förekomsten) av prostatit är 5-8%." Samma åsikter framförs HT 2004 i kursmateriel för utbildning av läkare inom Akuturologi, Karolinska Universitetssjukhuset, Solna. Detta innebär att så många som 250 000 män (från tonåren och uppåt) kan vara drabbade av sjukdomen i Sverige.
Prostatitis Prevalence, Austria Hochreiter W.W.1, Madersbacher S.2, Temml C.3, Zbrun S.1, Wolfensberger P.1, Studer U.E.1 1University of Bern, Department of Urology, Bern, Switzerland, 2Donauspital, Department of Urology, Vienna, Austria, 3City of Vienna, Department of Preventive Health, Vienna, Austria. INTRODUCTION & OBJECTIVES: To assess the prevalence of prostatitis-like symptoms and LUTS in an urban population and to determine possible risk factors. MATERIAL & METHODS: Men aged 20-80 years participating in a health- screening project in the area of Vienna completed the Chronic Prostatitis Symptom Index (CPSI) and the International Prostate Symptom Score (IPSS). In addition, all participants underwent a detailed health examination including physical assessment, evaluation of various life-style factors, medical history and blood analysis. RESULTS: A total of 1759 men were analysed. Overall, the median CPSI and IPSS values showed a slight increase with age from 2.5 and 1 in the 2nd decade of age to 5 and 7 in the 7th decade of age, respectively. Moderate to severe prostatitis symptoms (CPSI =9) were reported by 9% of all men: 5.4% (20-30 yrs.), 6.3% (31-40 yrs.), 8.5% (41-50 yrs.), 11.7% (51-70 yrs.) and 13% (71-80 yrs.). Men with more severe prostatitis symptoms also complained of more severe LUTS according to the IPSS. There was no statistically significant correlation between common risk factors such as diabetes, coronary heart disease, hypertension or overweight and the degree of LUTS and prostatitis symptoms. Neither stress nor consumption of alcohol, coffee or spicy foods were associated with the presence of LUTS and prostatitis symptoms. CONCLUSIONS: Overall, 9% of men in this study complained of moderate to severe prostatitis symptoms which were paralleled by LUTS. Apart from age, the comprehensive medical assessment was unable to identify well-defined risk factors.
Dr. Jack and Dr. Zeitlin: "Confronting Prostatitis" in Contemporary Urology. November 2004. p. 34 - 35. The
quote below is a good summary of the prevalence of prostatitis:
Inoue Y, Mita K, Kakehashi M, Kato M, Usui T Department of Urology, Graduate School of Medical Sciences, Hiroshima University, Hiroshima, Japan. AIMS: The aim of this study was to clarify the prevalence of painful bladder syndrome (PBS) symptoms in adult women in the general population in Japan. METHODS: Web-based survey through an internet-based market research company that enrolled 561,631 men and women in Japan was conducted from January 9 to January 11, 2007. After the women allocated to four age groups; 20s, 30s, 40s, and 50s or older, a total of 80,367 women, comprising an almost equal number from each age group, were then randomly invited to participate. The O'Leary and Sant symptom index was used as the questionnaire. The following classification was defined on the basis of the total points score: 0 to 3 points for negligible PBS symptoms, 4 to 6 points for mild symptoms, 7 to 11 points for moderate symptoms, and 12 to 20 points for severe symptoms. A category of possible cases of PBS was defined as severe PBS symptoms including nocturia (twice or more) and pain (2 points or more). RESULTS: A total of 32,074 women ranging in age from 20 to 88 years participated. 76.6% of respondents had negligible PBS symptoms, 17.3% had mild symptoms, 5.6% had moderate symptoms, and 0.5% had severe symptoms, respectively. The incidence rate of women with possible cases of PBS was 0.265% (85/32,074). CONCLUSIONS: Comparison with previous reports revealed no difference in the prevalence of PBS symptom in adult women in the general population between Japan and Western countries. Neurourol. Urodynam. 28:214-218, 2009. (c) 2009 Wiley-Liss, Inc.
Epidemiology of prostatitis: new evidence for a world-wide problem. Krieger JN, Riley DE, Cheah PY, Liong ML, Yuen KH. Department of Urology, University of Washington School of Medicine, VAPSHCS (112-GU), 1600 South Columbian Way, Seattle, WA 98108, USA. World J Urol 2003 Apr 24 Från
denna medicintidskrift saxar jag följande av intresse: Other epidemiologic data suggest that chronic prostatitis may be associated with an increased risk for development of benign prostatic hyperplasia and prostate cancer. These data suggest that chronic prostatitis is an important international health care problem that merits increased priority from clinicians and researchers.
Int J Antimicrob Agents. 2007 Dec 28 Krieger JN, Lee SW, Jeon J, Cheah PY, Liong ML, Riley DE. BACKGROUND: Prostatitis describes a combination of infectious diseases (acute and chronic bacterial prostatitis), chronic pelvic pain syndrome, and asymptomatic inflammation. MATERIALS AND METHODS: We employed evidence-based methods to review the epidemiology of prostatitis syndromes. RESULTS: The prevalence of prostatitis symptoms could be compared in five studies surveying 10617 men. Overall, 873 participants met various criteria for prostatitis, representing an overall rate of 8.2%, with prevalence ranging from 2.2 to 9.7%. A history of sexually transmitted diseases was associated with an increased risk for prostatitis symptoms. Men reporting a history of prostatitis symptoms had a substantially increased rate of benign prostatic hyperplasia, lower urinary tract symptoms and prostate cancer. In one study, the incidence of physician-diagnosed prostatitis was 4.9 cases per 1000 person-years. Two studies suggest that about one-third of men reporting prostatitis symptoms had resolution after 1 year. Patients with previous episodes and more severe symptoms are at higher risk for chronic pelvic pain. DISCUSSION: The prevalence of prostatitis symptoms is high, comparable to rates of ischaemic heart disease and diabetes. Clinical evaluation appears necessary to verify that prostatitis is responsible for patients' symptoms. Prostatitis symptoms may increase a man's risk for benign prostate hypertrophy, lower urinary tract symptoms and prostate cancer. We need to define natural history and consequences of prostatitis, develop better algorithms for diagnosis and treatment, and develop strategies for prevention.
Prostatitis prevalence and quality of life impact in 16-19 year-old north american males Dean A Tripp PhD, Stephanie Ross BA , Jennifer Pikard BS, Natalie Stechyson BA, Chris Mullins PhD and J Curtis Nickel MD ON, Canada.
INTRODUCTION AND OBJECTIVE: Prevalence and impact of chronic prostatitis in young men is unknown. This study examined prostatitis symptoms prevalence and the extent to which pain; urinary symptoms, depression and catastrophizing predict poorer Quality of Life (QoL) in males (16-19) years.
METHODS: Prostatitis–like symptoms prevalence in Canadian males was examined. Males was recruited from Queens University and the community. The Chronic Prostatitis Symptom Index (NIH-CPSI), Patient Health Questionnaire (PHQ-depression, anxiety) and the Pain Catastrophizing Scale (PCS) were completed. Prostatitis symptoms were defined as pain/discomfort in perineum and/or with ejaculation and total pain score 4 or greater. Prevalence was estimated and regression modeling examined predictors of poorer QoL from the NIH-CPSI.
RESULTS: Data was obtained from 264 Canadian males between the 16-19 years (M=17.6, SD=1.1) comprised of 160 from Queens, 104 from community. Overall. 67 (25.4%) of males reported a pain score of 4 or greater, and 18 (6.9%) a score of 8 or greater. Prevalence estimate of prostatitis symptoms was 8.3%. Further, 3% of this group reported a pain index score of 8 or greater. Hierarchical regression at step 1 showed an association between worse pain, urinary symptoms, and poorer QoL. In Step 2, depression and catastrophizing predicted QoL after controlling for pain and urinary symptoms, R2 change= .03, F(2,259) = 53.07, p< .001. In the final model, only pain, urinary symptoms and catastrophizing predicted poorer QoL. Catastrophizing was the unique psychological predictor of QoL while pain was the strongest predictor of poorer QoL.
CONCLUSIONS: A prevalence of 8.3% in young males warrants concern, especially when 3% reported mod-severe symptoms. This novel report suggests pubertal male report symptoms similar to current estimates in older age cohorts, which have a negative impact on current QoL. Experiencing prostatitis-like symptoms younger in life may be a risk for development of chronic prostatitis/chronic pelvic pain syndrome. These findings suggest that the normal history of disease progression from a juvenile patient cohort with prostatitis-like symptoms to adults with reported chronic prostatitis/chronic pelvic pain syndrome is an important and understudied area for future investigations.
Abstract från AUA möte 2008-05-17.
Results from the Boston area community health (bach) survey Nicholas A. Daniels, San Francisco, CA; Carol L. Link, Watertown, MA; Michael J. Barry, Boston, MA; John B. McKinlay, Watertown, MA. Prostatitis symptoms occur in about 5 % of men age 30 to 79 years and correlate strongly with a history of urinary tract infection (UTI) and age, according to an analysis of the Boston Area Community Health (BACH) survey. Race - black, white, Hispanic - and socioeconomic status make no difference. This analysis included the first 1,559 men that age who answered questionnaires, which included pain and urinary symptom questions from the NIH-CPSI. Of those men, 79 reported symptoms. Among those age 30 to 39 years, 1.22 % had symptoms; of those 40 to 49, 2.21 % had symptoms; in the 50 to 59 group, 8.08 % had symptoms; and in the 60 to 79 group, 7.72 % had symptoms. That meant that 30- to 39-year-olds had 0.16 times the odds of 60- to 79-year-olds of having prostatitis symptoms. Of men who had had a UTI, 12.60 % had prostatitis symptoms versus 2.98 % who had not had UTIs, giving those who had UTIs 3.8 times greater odds of having prostatitis symptoms.
BJU Int. 2003 Dec;92(9):955-9. Rizzo M, Marchetti F, Travaglini F, Trinchieri A, Nickel JC. Department of Urology, University of Florence, Florence, Medical Department, GlaxoSmithKline S.p.a, Verona, Clinics of Urology, University of Milan, Milan, Italy, and Queen's University, Kingston, Canada. OBJECTIVE: To report a prospective, multicentre descriptive study designed to determine the prevalence of the diagnosis of prostatitis in male outpatients examined by urologists in Italy, and to further examine the diagnostic evaluation and treatment of patients identified with a clinical diagnosis of prostatitis. PATIIETS AND METHODS: Between July 2001 and October 2001, 70 urologists, representing a cross-section of urological centres in Italy, counted and recorded the overall total of men reported in the clinic and that of patients diagnosed with prostatitis over a 5-week period. Data on demographics, previous diagnoses, symptoms, physical examination, laboratory data and therapy instituted were collected. Patients with a diagnosis of prostatitis completed questionnaires on symptom frequency and severity, and quality of life. RESULTS: In all, 8503 patients were included in the primary outcome analysis; 1148 were identified with prostatitis (12.8%; mean age 47.1 years, range 16-83) with all age ranges equally represented, and 68% had had their first symptom within the last year. The most common presenting symptoms were severe, bothersome urinary frequency, obstructive voiding symptoms, perineal, suprapubic and penile pain or discomfort. The self-administered questionnaire confirmed that the most frequently reported and most severe symptoms at the time of evaluation were irritative voiding symptoms, perineal and suprapubic pain and discomfort. Over three-quarters of the patients were dissatisfied with their quality of life. While 98% of the patients had a digital rectal examination and expressed prostatic secretion was successfully recovered in 44%, < 3% of the patients had the traditional Meares-Stamey four-glass test. The most common treatment prescribed was drug therapy. CONCLUSION: The prevalence of a clinical diagnosis of prostatitis in urology outpatient practice in Italy was 12.8%. The prevalence, diagnosis, evaluation and treatment of prostatitis reported in this prospective study was very similar to that reported in other retrospective series from other countries.
J Urol 2005;174:581-3 Leppilahti M, Sairanen J, Tammela TL, Aaltomaa S, Lehtoranta K, Auvinen A; Finnish Interstitial Cystitis-Pelvic Pain Syndrome Study Group. Division of Urology, Seinajoki Central Hospital, Seinajoki, Department of Urology, Helsinki University Hospital, Helsinki, Finland. mikael.leppilahti@epshp.fi PURPOSE: Interstitial cystitis (IC) is a clinical condition occurring predominantly in women that is characterized by irritative voiding symptoms, including urinary frequency, urgency and pain. To our knowledge its etiology is unknown and little is known about its occurrence. We evaluated the prevalence of IC in women in Finland. MATERIALS AND METHODS: A total of 2,000 participants were randomly selected from the Finnish population register. Urinary symptoms were evaluated using the validated O'Leary-Sant IC symptom and problem index questionnaire. Women with moderate or severe symptom scores (7 or higher) without any urinary tract infection during the last month were invited to undergo clinical examination. RESULTS: Of the 1,331 respondents 32 had moderate or severe symptoms involving a suspicion of IC, of whom 21 underwent clinical evaluation. Three women were found to have probable IC and 4 had possible IC. Thus, the prevalence of clinically confirmed probable IC in women was 230/100.000 (95% CI 100 to 360) and that of possible/probable IC was 530/100.000 (95% CI 140 to 910). Considering the lack of information on 8 patients with urinary symptoms the corrected estimates were 300/100,000 (95% CI 120 to 770) and 680/100,000 women (95% CI 360 to 1,300), respectively. CONCLUSIONS: Our results based on a large and representative population, and clinically confirmed diagnoses indicate that IC is substantially more common than previously thought.
Tillbaka till Allmänt om sjukdomen (på sidan Interstitiell Cystit)
Ibrahim
IA, Diokno AC, Killinger KA, et al. Int Urol Nephrol 2007 Mar 13; [Epub
ahead of print] William Beaumont Hospital, Royal Oak, MI, USA, iibrahim@beaumont.edu. PURPOSE: Reported estimates of IC prevalence vary widely. The objective of this study is to determine the prevalence of IC among community-dwelling adult women. METHODS: We analyzed survey responses from 215 established IC cases and 823 age-matched community-dwelling controls. Using a history of diagnosis of urinary conditions and presence of pelvic pain within the last six months, we identified those with possible IC among the controls using various operative definitions. RESULTS: The prevalence rates of self-reported IC (SRIC) and IC-like symptoms (ICLS) among controls in the community were 3.7% and 4.4%, respectively. Expanding ICLS by including women who reported pelvic pain only raised the prevalence to 17.3%. CONCLUSIONS: According to our prevalence rates and population estimates in the United States census 2000, the number of adult women who possibly have interstitial cystitis is estimated to be between 422,803 and 21,454,813. Although estimates based on the question of having ever been diagnosed with IC lead to an estimate close to that derived from symptoms, underestimation of IC prevalence might occur in the absence of additional questions and testing to validate and qualify the responses further. There is also a need for clinical studies to verify and validate the diagnoses to enable accurate assessment of the sensitivity and specificity of such history survey questions.
Interstitial cystitis: current issues and controversies in diagnosis Urology [the Gold Journal] 2001 Jun;57(6 Suppl 1):82-8. Sant GR, Hanno PM. Department of Urology, Tufts University School of Medicine, Interstitial Cystitis Center, New England Medical Center, Boston, Massachusetts 02111, USA. Mail: gsant@lifespan.org Up to 70% of men with symptoms of nonbacterial prostatitis and prostatodynia have the cystoscopic appearance (NIH-NIDDK criteria) of IC when cystoscoped under anesthesia.[34 and 35] This raises the possibility that IC in men frequently masquerades as nonbacterial prostatitis/prostatodynia. The recent classification of the type 3 prostatitis syndrome as chronic pelvic pain syndrome (inflammatory and noninflammatory) suggests that IC and chronic bacterial prostatitis/prostatodynia may be the same syndrome. [34 and 35] The symptoms in both conditions are similar, including irritative voiding symptoms, pain (pelvic, bladder, prostate, genital), sexual dysfunction, and the comorbidities of depression and anxiety. In a pilot open-label study, sodium pentosan polysulfate (a drug used to treat IC) reduced the severity and frequency of voiding symptoms and pain, and improved the quality of life in men with the chronic pelvic pain syndrome. [36]. CPP may be the primary symptom of IC. Such patients with bladder pain, dyspareunia, and perimenstrual symptom exacerbation are frequently referred for gynecologic evaluation whereas patients with bladder irritability present to urologists and gynecologists with symptoms of the overactive bladder and are treated with oral anticholinergics. IC is a common cause of CPP in women.[11 and 37] A significant percentage of women with CPP remain undiagnosed after full gynecologic evaluation. Laparoscopic evaluation in this group of patients is negative or reveals microscopic endometriosis. These data strongly suggest that gynecologists, urogynecologists, and primary care physicians need to consider IC in the differential diagnosis of CPP in women.
Samband mellan kronisk prostatit och reumatism, Colombia Enligt Dr. Fernando Valero Cely Profesor Asociado - Departamento de Cirugía - Unidad de Urología, Dr. Carlos Guzmán Bastidas Profesor Asistente - Departamento de Cirugía - Unidad de Urología Universidad Nacional de Colombia. Från hemsidan http://www.encolombia.com/medicina/urologia/urologia11302-prostatitis.htm citerar jag följande: "Las enfermedades reumáticas han sido reportadas entre el 21 % y 29 % de los pacientes con prostatitis Categoría III y en el 3 % de estos hay antecedentes familiares de Cistitis Intersticial. Esto podría también sugerir algún proceso inmunológico como factor etiológico." Översatt till engelska: Rheumatic diseases have been reported between 21 % and 29 % of the patients with prostatitis Category III (Chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CPPS), where there is no demonstrable infection) and in 3 % of these are familiar antecedents of Interstitial Cystitis. This could also suggest some immunological process as an etiologic factor.
Mycoplasmas in semen of chronic prostatitis patients Från Scandinavian Journal of Urology and Nephrology December 2005 , pages 479 - 482. Reet Mändar; Elve Raukas; Silver Türk, Paul Korrovits; Margus Punab.Department of Microbiology, University of Tartu. Tartu. Estoni, OÜ Quattromed. Tartu. Estonia, Andrology Unit, Tartu University Clinicum. Tartu. Estonia Abstract Objective: To evaluate the occurrence of mycoplasmas in the semen of chronic prostatitis patients. Material and methods: Genital mycoplasmas (Mycoplasma hominis, Mycoplasma genitalium, Ureaplasma urealyticum, Ureaplasma parvum) were sought in the semen of 121 chronic prostatitis patients [38 National Institutes of Health (NIH) category IIIa, 59 NIH category IIIb and 24 NIH category IV] and 40 controls. The commercially available kit Mycoplasma IST was applied to the semen samples of all 161 men, and polymerase chain reaction (PCR) to those of 60 randomly selected men. Results. Ureaplasmas were found in all study groups (at frequencies ranging from 12% to 25%) using the Mycoplasma IST test, but M. hominis was found only in one NIH category IIIb patient. Using PCR, most of the ureaplasmas appeared to be U. parvum, which was found in all prostatitis groups (18% of NIH category IIIa, 15% of NIH category IIIb and 25% of NIH category IV patients) but not in the controls. M. genitalium was found in 18% of the NIH category IIIa patients. All of the mycoplasmas occurred significantly more frequently in prostatitis patients than in controls and in NIH category IIIa patients than in controls. Conclusion: Mycoplasmas occur more frequently in the semen of prostatitis patients than in that of healthy controls, with U. parvum being the most frequently occurring species. Hela artikeln finns på http://www.informaworld.com/smpp/content~content=a727443216?words=prostatitis&hash=2387638923
Predictors of symptom severity in patients with chronic prostatitis and interstitial cystitis Journal
of Urology, March. 2006. PURPOSE: Numerous studies have been performed to identify potential risk factors for CP/CPPS and IC. However, few studies have been done to identify predictors of disease severity. MATERIALS AND METHODS: A total of 174 men with CP/CPPS and 111 women with IC completed questionnaires to quantify symptom severity and identify demographic, medical and psychosocial characteristics. Symptom severity was assessed with the National Institutes of Health CPSI in men, and the O'Leary-Sant ICSI and problem index in women. Univariate and multivariate analyses were performed to identify characteristics predictive of worse symptoms. RESULTS: The mean National Institutes of Health CPSI score in men was 15.32, and the mean O'Leary-Sant ICSI and problem index in women was 19.17. The most commonly reported comorbidities were allergies, sinusitis, erectile dysfunction and irritable bowel syndrome in men. Allergies, urinary incontinence, sinusitis and irritable bowel syndrome in women. In the 2 sexes self-reported urinary frequency and urgency, worse depression scores and lower education level were independent predictors of worse symptom severity. In men additional independent predictors were self-reported pelvic pain, fibromyalgia and previous heart attack, and in women an additional independent predictor was postmenopausal status. CONCLUSIONS: There are several common medical conditions associated with urological pelvic pain syndromes in men and women. Few of them were predictive of symptoms severity in this analysis. Self-reported pelvic pain symptoms, education and depression severity were the factors most strongly predictive of symptom severity in patients with CP/CPPS and IC.
Prevalence of chronic prostatitis in men with premature ejaculation, Italien. Urology 2001 Aug;58(2):198-202 Screponi E, Carosa E, Di Stasi SM, Pepe M, Carruba G, Jannini EA. Division of Medicine of Reproduction and Sexology, Department of Experimental Medicine, University of L'Aquila, L'Aquila, Italy. Objectives: To investigate the prevalence of chronic prostatitis in men with premature ejaculation. The etiology of premature ejaculation is currently considered psychological in nature. However, the possibility that urologic, hormonal, or neurologic factors may contribute to this condition should be considered in its management. Methods: We evaluated segmented urine specimens before and after prostatic massage and expressed prostatic secretion specimens from 46 patients with premature ejaculation and 30 controls by bacteriologic localization studies. The incidence of premature ejaculation in the subjects with chronic prostatitis was also evaluated. Results: Prostatic inflammation was found in 56.5% and chronic bacterial prostatitis in 47.8% of the subjects with premature ejaculation, respectively. When compared with the controls, these novel findings were statistically significant (P <0.05). Conclusions: Considering the role of the prostate gland in the mechanism of ejaculation, we suggest a role for chronic prostate inflammation in the pathogenesis of some cases of premature ejaculation. Since chronic prostatitis has been found with a high frequency in men with premature ejaculation, we stress the importance of a careful examination of the prostate before any pharmacologic or psychosexual therapy for premature ejaculation.
Prevalence of premature ejaculation in Turkish men with chronic pelvic pain syndrome Journal of Andrology 2005 Sep-Oct. Gonen M, Kalkan M, Cenker A, Ozkardes H. Baskent Universitesi Konya Arastirma ve Uygulama Merkezi, Hocacihan mah Saray cad no:1, Selcuklu, Konya, Turkey . mgonen01@hotmail.com. Chronic pelvic pain syndrome is a common and serious health problem affecting the quality of life in men. Limited studies exist on the relation of this condition to premature ejaculation. We evaluated prevalence rates of premature ejaculation in Turkish male patients with chronic pelvic pain syndrome and compared them with healthy control subjects. Sixty-six men with chronic pelvic pain syndrome were included in the study (group 1). A questionnaire consisting of 2 parts-demographic data and a Turkish version of the National Institutes of Health Chronic Prostatitis Symptom index-was administered to all patients. Premature ejaculation was defined as intravaginal ejaculation latency of less than 2 minutes with the same partner for at least 6 months. All patients were evaluated with physical examinations and routine laboratory tests. If erectile dysfunction was noted from the medical history, penile Doppler ultrasonography also was performed. The results were compared with the results of 30 healthy men without urinary symptoms (group 2). The chi(2) test was used for statistical analyses. Of 66 patients with chronic pelvic pain syndrome, 51 had premature ejaculation (77.3%), and in 10 (15.2%) patients, premature ejaculation and erectile dysfunction were found together. Penile Doppler ultrasonography showed no vascular pathology in patients with erectile dysfunction. The rate of premature ejaculation was higher in patients in the study group than it was in patients in the control group, and this difference was statistically significant (P < .05). Both chronic pelvic pain syndrome and premature ejaculation are common disorders, but their ethiopathogeneses are not well understood. In Turkish men with chronic pelvic pain syndrome, the incidence of psychogenic sexual problems was higher than in the normal population.
Ejaculatory pain affects 75% of men with CPPS UROLOGY TIMES, July 2004, Penny Allen UT correspondent. San Francisco - Post-ejaculatory pain is understood to be a variable feature of chronic prostatitis/chronic pelvic pain syndrome. But until now, no study had addressed how common it is, what might cause it, or the implications for future study and treatment. Examining data from the National Institutes of Health Chronic Prostatitis Cohort Study, Daniel A. Shoskes, MD, and colleagues found that about three-fourths of men with chronic pelvic pain syndrome always have post-ejaculatory pain, and that these men have more severe prostatitis symptoms overall. In addition, the researchers found no indication that ejaculatory obstruction, occult infection, or worse inflammation was responsible. Dr. Shoskes and his team analyzed the answers to questionnaires given to 486 men with chronic pelvic pain at baseline and at each of three monthly follow-up contacts. The men were divided into subgroups based on whether they never had post-ejaculatory pain (128 patients); did not have it at the beginning of the study, but pain appeared later (106); had pain at the beginning of the study, but not later (137); or have always had pain (115). The men’s symptoms, quality of life, and sexual practices were examined, as were blood cell counts for bacterial growth. Patients’ symptom scores (NIH Chronic Prostatitis Symptom Index total score, excluding post-ejaculatory pain) increased progressively through the four groups: 18.5 for the men who never had post-ejaculatory pain through 25.5 for those who always had pain—a highly significant difference (p<.0001). Mental and physical quality-of-life scores went progressively down through the subgroups from no post-ejaculatory pain to those who always had it. Men who always had post-ejaculatory pain were about 5 years younger than men in the other groups; more likely to live alone; had lower incomes; and had a tendency to have a greater variety of sexual practices. However, none of these were statistically significant. There were no significant differences in white blood cell counts or bacterial growth in urine, prostate fluid, or semen. What has struck me is that you can have patients with identical presentations, history, everything the same. But some have severe post-ejaculatory pain and try to avoid ejaculating at all costs, and others, not only do they have no pain, but their symptoms are relieved when they ejaculate,” said Dr. Shoskes, chairman of the department of kidney transplantation, Cleveland Clinic Florida, Weston. Obstruction ruled out Dr. Shoskes said many have speculated on the reasons why, hypothesizing that those with pain have infections or obstruction. But Dr. Shoskes found no difference in ejaculatory volume between groups and ruled out obstruction as a cause of postejaculatory pain. Finding no differences in the presence of either common bacteria or organisms responsible for sexually transmitted diseases such as chlamydia showed that infection wasn’t responsible for this symptom either. “Unfortunately, the study doesn’t point to positive choices for treatment. But it does point to negative choices,” he said. “In other words, the fact that the person has post-ejaculatory pain does not mean they necessarily have an infection.” That the men who have this symptom all the time also do much worse than others has important implications for clinical research, Dr. Shoskes said. “ Asking about [the presence of postejaculatory pain] is an important variable to stratify for when designing new clinical trials,” he said. Dr. Shoskes “The fact that the person has post-ejaculatory pain does not mean they necessarily have an infection.”
Infertilitet (infertility) orsakad av kronisk prostatit I västvärlden anses infertilitet förekomma hos 10-15 % bland fasta relationer som försöker skaffa barn. Beror på flera olika orsaker. I mannens fall pekar olika studier på att prostatit kan vara en orsak.
Chlamydia trachomatis infection as a problem among male partners of infertile couples Ouzounova-Raykova V, Ouzounova I, Mitov I. Department of Microbiology, Medical University of Sofia, Sofia, Bulgaria. pumpi@abv.bg Chlamydia trachomatis infection is the most common bacterial sexually transmitted disease supposed to cause urethritis, epididymitis, prostatitis and infertility in men. The objective of this study was to assess the frequency of C. trachomatis infection in male partners of infertile couples at childbearing age. Sixty infertile couples and a control group of 40 healthy volunteers were included in the study. Urethral swabs were taken from all the male participants and cervical swabs from the female partners of the infertile couples. Culturing on McCoy cell line and PCR were the methods used for detection of the infection. C. trachomatis was found in five out of the 60 male urethral samples. Three of the female partners of these five positive males were diagnosed with C. trachomatis infection, too. We registered a woman with C. trachomatis infection whose partner's samples were negative for the bacterium. The control group showed one specimen positive for C. trachomatis. The frequency of C. trachomatis infection was 8.3% in the male partners of infertile couples at childbearing age when compared with 2.5% in the control group. It is most likely that infertility in the couples with chlamydial infection was due to the pathogen studied. Se http://www.ncbi.nlm.nih.gov/pubmed/19143724
Environmental Factors Influence Development of Chronic Prostatitis Symptoms, Korea Urology 2001;58:853-858 NEW YORK (Reuters Health) Jan 16, 2002 - Lower education levels and less exposure to sunlight are linked to the development of chronic prostatitis-like symptoms, according to a report by Korean investigators. Previous studies have yielded conflicting results regarding the impact of heat or sunlight exposure on the risk of chronic prostatitis. To better understand possible environmental factors, Dr. Ja Hyeon Ku, from the Military Manpower Administration in Taejeon, and colleagues conducted an epidemiologic study of 16,321 community-dwelling men who were 20 years of age. Six percent of men had significant chronic prostatitis-like symptoms, the authors report in the December issue of Urology. On univariate analysis, education level, average duration of sunlight, and average temperature were inversely linked to the risk of developing prostatitis-like symptoms. Multivariate analysis revealed that men with no more than a middle school or high school education were 1.8 and 1.4 times more likely, respectively, to develop prostatitis-like symptoms than men who attended college. Duration of sunlight was confirmed as an independent risk factor on multivariate analysis, but average temperature lost its significance. The current findings indicate that the prevalence of chronic prostatitis-like symptoms in community-dwelling young men is high, the researcher note. In this group, higher education levels and longer exposure to sunlight are tied to a reduced risk of chronic prostatitis-like symptoms, they conclude.
A case-control study of risk factors in men with chronic pelvic pain syndrome BJU Int. 2005 September. Pontari MA, McNaughton-Collins M, O'leary MP, Calhoun EA, Jang T, Kusek JW, Landis JR, Knauss J, Litwin MS; The CPCRN Study Group.Temple University, Philadelphia, PA, USA. OBJECTIVE: To compare the demographic, behavioural, clinical and medical history characteristics of men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and asymptomatic controls, to identify characteristics that might be associated with this syndrome. PATIENTS AND METHODS: Self-administered epidemiological questionnaires were completed by 463 men with CP/CPPS and 121 asymptomatic age-matched controls. We compared the prevalence of possible risk factors between men with CP/CPPS and controls, using generalized Mantel-Haenszel tests, and developed multivariate predictive models using logistic regression methods, adjusting for clustering by clinical centre within both methods. RESULTS: Compared to controls, men with CP/CPPS reported a significantly greater lifetime prevalence of nonspecific urethritis (12% vs 4%, P = 0.008), cardiovascular disease (11% vs 2%, P = 0.004), neurological disease (41% vs 14%, P < 0.001), psychiatric conditions (29% vs 11%, P < 0.001), and haematopoietic, lymphatic or infectious disease (41% vs 20%, P < 0.001). CONCLUSION: A wide range of self-reported medical conditions was associated with CP/CPPS. Further studies are necessary to determine whether they play a role in the pathogenesis of CP/CPPS.
A. Mehik, P. Hellström, A. Sarpola, O. Lukkarinen and M.-R. Järvelin Division of Urology, Department of Surgery, Oulu University Hospital, Department of Public Health Science and General Practice, Oulu University, Oulu, Finland, and Department of Epidemiology and Public Health, Imperial College School of Medicine, University of London, London, UK Objective: To determine the occurrence of mental distress related to prostatitis in Finnish men. Subjects and methods: A population-based cross-sectional survey was conducted of 2500 men aged 20-59 years living in the two northernmost provinces of Finland (Oulu and Lapland). The final response rate was 75% (1832 men). Results: The fear of undetected prostate cancer was reported by 17% of the men in the population who had had prostatitis, a value significantly higher (P < 0.001) than in healthy men. Fears of having a sexually transmitted disease and suicidal thinking were also slightly more common. The men who had had prostatitis preferred to be alone in a public toilet during voiding (58% vs 44%, P < 0.001). Erectile dysfunction was reported by 43% of the men with symptomatic prostatitis and decreased libido by 24%. Self-assessment of personality, adjusted for age, showed that the men with prostatitis were more often busy and nervous than the healthy controls (P < 0.001), and that they had a more meticulous attitude to life and its problems. Marital difficulties were reported by 17% of the men who had had prostatitis at some point in their lives, and 4% were convinced that their illness had caused their divorce. Socio-economic status and social well-being had no apparent influence on the occurrence of prostatitis. Conclusions: This survey showed that psychological stress is common in men with prostatitis. Urologists and general practitioners should consider that a consultation with a psychiatrist may be appropriate for selected men with prostatitis.
Tillbaka till Symtom (på sidan Prostatasjukdomarna)
Clemens JQ, Brown SO, Calhoun EA Department of Urology, University of Michigan Medical Center, Ann Arbor, Michigan 48109-5330, USA. qclemens@umich.edu PURPOSE: We compared the rate of mental health disorders in male and female patients with pelvic pain and control subjects. MATERIALS AND METHODS: Male patients with chronic prostatitis/chronic pelvic pain syndrome (174) and female patients with interstitial cystitis/painful bladder syndrome (111) were identified from a urology tertiary care clinic population. A control group consisting of 72 men and 175 women was also recruited. Subjects completed self-administered questionnaires that included items about demographics, medical history, medication use and urological symptoms. The Patient Health Questionnaire was used to identify depression and panic disorder. Multiple logistic regression was used to determine odds ratios for the presence of a mental health diagnosis. RESULTS: Mental health disorders were identified in 13% of the chronic prostatitis/chronic pelvic pain syndrome cases and 4% of male controls (OR 2.0, p = 0.04), as well as in 23% of interstitial cystitis/painful bladder syndrome cases and 3% of female controls (OR 8.2, p <0.0001). Disease status (case vs control) (OR 10.4, p = 0.001) and income greater than $50,000 (OR 0.34, p = 0.008) were the only 2 variables independently predictive of the presence of a mental health diagnosis. Age, gender, race/ethnicity and education were not predictive. Medications for anxiety, depression or stress were being taken by 18% of patients with chronic prostatitis/chronic pelvic pain syndrome, 37% of those with interstitial cystitis/painful bladder syndrome, 7% of male controls and 13% of female controls. CONCLUSIONS: Depression and panic disorder are significantly more common in men and women with pelvic pain conditions than in controls. Medication use data suggest that anxiety and depression may be more difficult to treat in patients with urological pain syndromes than in controls.
National Institute of Public Health and The Urology Clinic FN Hradec Kralove, Tjeckien. Statistical analysis performed by Jiri Jerabek, M.D., Ph.D. The urological study performed by P. Navratil, M.D. 1997. Chronic inflammatory affection of prostate-vesicle-urethral complex is one of most extensively studied urological problem. About 10-15% of young and middle age men suffer from this disease.As the consequence disturbances of reproduction and sexual life are observed in almost all of them. As human sexuality is closely bound to the psychic sphere, most of patients end at the psychiatric departments. From this viewpoint this disease is not only a medical but a social problem as well. Because the etiology remains unclear, treatment is extremely difficult. Three leading syndromes are recognized: algic, sexual dysfunctional and irritation dysfunctional. Therapy must always be complex including changes of life habits, drugs, physiotherapy, psychotherapy, and balneotherapy. Regardless of this complex approach, according to our observations about 50 % of patients are highly stigmatised and about 20 % of them are invilidated. Due to our experience we feel that we are obliged to prove any new therapeutically approach (Pulsed magnetic field in therapy of Prostatitis) having a chance to be successful. e-mail: 2ELinfo@czechia.com och URL: http://www.czechia.com/2el/prostudy.htm
Tillbaka till Behandling (På sidan Prostatasjukdomar)
Int J Urol. 2003 Dec;10(12):636-642 Kiyota H, Onodera S, Ohishi Y, Tsukamoto T, Matsumoto T. Department of Urology, Jikei University, Tokyo, Sapporo Medical University, Sapporo and University of Occupational and Environmental Health, Kitakyushu, Japan. OBJECTIVES: We performed a questionnaire survey to investigate various issues in the diagnosis and treatment of chronic prostatitis/chronic pelvic pain syndrome by Japanese urologists and to clarify the circumstances surrounding prostatitis in Japan. METHODS: Japanese urologists (n = 1869) were surveyed by mail using a 17-item questionnaire to determine current diagnostic and treatment practices for prostatitis/chronic pelvic pain syndrome. RESULTS: Only 1.5% (11/739) of urologists diagnosed chronic prostatitis/chronic pelvic pain syndrome using the 4-glass test, while most did so using the 2-glass test (voided bladder [VB]2 and VB3, or VB2 and expressed prostatic secretion [EPS]). pproximately half (55.2%; 412/746) did not perform urine cultures to differentiate chronic bacterial prostatitis from chronic abacterial prosta itis/chronic pelvic pain syndrome. Approximately half (46%; 343/746) did not count the number of leukocytes in VB2 or VB3/EPS to differentiate chronic abacterial prostatitis from chronic pelvic pain syndrome. Although many urologists (63.8%; 459/720) thought that chronic abacterial prostatitis/chronic pelvic pain syndrome was not an infectious disease, many chose antimicrobial agents as the primary treatment. More than half (52.2%; 384/735) of all urologists felt pessimistic about dealing with chronic prostatitis/chronic pelvic pain syndrome compared to treating benign prostatic hypertrophy or prostate cancer, because of the high number of complaints by patients and their own lack of confidence in diagnosing and treating the condition. CONCLUSION: There is much confusion and frustration among Japanese urologists about chronic prostatitis/chronic pelvic pain syndrome. Further studies are needed to elucidate its etiology and pathogenesis, and to establish guidelines for its diagnosis and treatment.
Sunpunkter på behandlingsresultat från kinesiska urologer BJU Int. 2004 Sep;94(4):568-70. An epidemiological study of patients with chronic prostatitis. Liang CZ, Zhang XJ, Hao ZY, Yang S, Wang DB, Shi HQ, Liu C. Department of Urology, the First Affiliated Hospital of Anhui medical University, Hefei, China. OBJECTIVE: To assess possible causes, clinical symptoms and improvements in treatment for chronic prostatitis in China. PATIENTS AND METHODS: The study comprised 3000 patients with chronic prostatitis (aged 20-59 years), selected from urological clinics at province, city and county levels in Anhui (a province in mid-eastern China). Anonymous questionnaires were distributed which included 29 items to ascertain patient age, height, weight, educational background, personality, career, disease course, treatment status, prostatic fluid test and score of the National Institute of Health Chronic Prostatitis Symptom Index (NIH-CPSI). RESULTS: In all, 2498 valid questionnaires were collected (response rate 83.3%); 78.2% of the patients were aged <40 years and there were fewer patients in groups of increasing age. Discomfort and pain in the pelvis was reported by 52.3%, pain on urination by 23.0%, sexual discomfort by 21.8%, urinary frequency by 65.8%, and voiding discomfort by 74.4%; 34.9% of men were satisfied with their previous treatment. ISOPs kommentar: Detta innebär, att cirka 65 % inte fick någon hjälp av behandlingen! CONCLUSION: In China there are fewer patients with chronic prostatitis as age increases. The main symptoms were voiding dysfunction, e.g. frequent urination. The prevalence of pain, e.g. on urination, was significantly less than documented in other parts of the world. Most patients had used antibiotics to treat their prostatitis; generally the effect of treating prostatitis was unsatisfactory. Se även Asian Journal of Andrology http://www.nature.com/aja/journal/v11/n2/full/aja200846a.html
Behandlingsresultat vid prostatit enligt en studie av amerikanska NIH
Behandlingsresultat vid prostatit enligt en studie av the National Institutes of Health (USA).
Andreas E. Reissigi, Bregenz, Austria; Bob Djavan, Vienna, Austria; Josef Pointner, Stefan Obwexer, Bregenz, Austria Men with CPPS and no evidence of inflammation (type IIIB) who had been in a trial of treatment with Permixon (Serenoa repens or saw palmetto) were re-evaluated 3 years after their treatment. Although they had improvements at 6 and 12 months during the trial, those effects didn't last over the long term after therapy was discontinued. Fifty-five of the 72 men in the original study answered the NIH-CPSI questionnaire. By 6 months, 78.2 % of the men had at least mild (30 % to 50 %) improvement, and 71.8 % did at 12 months, but only 32.5 % showed that degree of improvement 3 years later. Also, by 6 months in the original study, 42.5 % of the men had significant (50 % or better) improvement, and by 12 months, 44.2 % did, but only 19 % had that level of improvement 3 years later. Short-term monotherapy doesn't have a continuous effect in CPPS patients, the researchers concluded. En
liknande studie http://www.therubins.com/illness/Prostatit.htm
presenterades i USA 2006-02-17: About 2.5 million American males take the herbal supplement saw palmetto for their enlarged prostate problem. Saw palmetto is an extract from the berry of the American dwarf palm tree, common in Florida and the southeastern part of this country. The National Institutes of Health sponsored the study. It is estimated that more than half of all Americans over 29 years of age suffers from BPH. A recent study concluded that the supplement was no more helpful in alleviating the problem than was a placebo. The multistudy analysis was performed by the Cochrane Collaboration, a nonprofit group that specializes in reviewing medical literature. Stephen Bent, professor of medicine at the University of California, San Francisco, was the main author of the study. Patients took the capsules for a year. Symptoms were assessed through a questionnaire and by measuring of the size of the prostate gland and the volume of urine left, as well as other tests. The study found no significant difference between the placebo and the saw palmetto group. A prior study analysis of 21 trials involving over 3,000 men found that the saw palmetto did provide "mild to moderate improvement" in symptoms with fewer adverse events than finasteride.
Many Patients with CPPS Symptoms May Have Infection Skerk V, Caji V, Markovinovi L, Rogli S, Zekan S, Skerk V, Radosevi V, Tambi Andragevi A. Etiology of chronic prostatitis syndrome in patients treated at the university hospital for infectious diseases "Dr. Fran Mihaljevi" from 2003 to 2005. Coll Antropol. 2006 Dec;30 Suppl 2:145-9. At an outpatient clinic in Croatia, nearly 60% of patients with symtoms of chronic prostatitis syndrome (CPPS) had infection. The clinicians said that, of 835 patients, 482 (57.72%) had pathogens causing the symptoms. Those included Chlamydia trachomatis in 161 patients, Trichomonas vaginalis in 85, Escherichia coli in 68, Enterococcus in 51, Proteus mirabilis in 20, Klebsielia pneumoniae in 9, Streptococcus agalactiae in 15, Ureaplasma urealyticum in 49, and mixed infection in the remainder. About half (257 or 53.3%) these patients had white blood cells in their expressed prostatic secretions or from urine collected after the secretions are expressed. Had infection not been found, this would have categorized these men's disease as type 3a prostatitis. Of the 161 patients who had infection with C trachomatis, 103 (63.98%) did not show excessive white blood cells in their specimens. That was also true in 50 (58.82%) of the 85 patients with T vaginalis and in 23 (46.94%) of 49 patients with U urealyticum. These findings may imply that CPPS may be misdiagnosed, and men may, in fact, have an infection, that is, type 1 prostatitis.
J Chemother 2002 Aug;14(4):384-9 Skerk V, Schonwald S, Krhen I, Markovinovic L, Barsic B, Marekovic I, Roglic S, Zeljko Z, Vince A, Cajic V. A total of 123 patients, older than 18 years of age, with symptoms of chronic prostatitis and inflammatory findings as well as the presence of Chlamydia trachomatis confirmed by DNA/RNA DIGENE hybridization method in expressed prostatic secretion or in voided bladder urine collected immediately after prostatic massage, were examined. The patients were randomized to receive a total of 4.5 g of azithromycin for 3 weeks, given as a 3-day therapy of 1 x 500 mg weekly or clarithromycin 500 mg b.i.d. for 15 days. Patients' sexual partners were treated at the same time. Clinical and bacteriological efficacy were evaluated 4-6 weeks after the end of therapy. In the group of patients with chronic chlamydial prostatitis the eradication rates (azithromycin 37/46, clarithromycin 36/45) and the clinical cure rates (azithromycin 32/46, clarithromycin 32/45) were not significantly different with regards to the administered drug (p > 0.05). In the group of patients with asymptomatic chlamydial prostatitis the eradication rates (azithromycin 11/16, clarithromycin 10/15) were not significantly different with regards to the administered drug (p = 1.00, OR = 1.1).
Från: Eur Urol. 2004 Nov; 46(5):647-50 2004-11-30 BERKELEY, CA (UroToday Inc.) - Chlamydia trachomatis is the most common sexually transmitted disease agent worldwide and is known to be one of the etiological microorganisms of chronic prostatitis. Doxycycline and azithromycin are the most widely prescribed drugs in the treatment of C. trachomatis infections and are often recommended for primary treatment, with the flouroquinolones recommended as alternative drugs. Antibacterial susceptibility against chlamydial organisms isolated from patients has proven variable however. Little is known, for example, about chlamydial survival in the presence of flouroquinolones in patients being treated for bacterial prostatitis. To clarify this point, activity of four flouroquinolones, as well as azithromycin and doxycycline were investigated and compared in vitro against C. trachomatis isolated from urethral and prostatic fluid culture of patients with chronic prostatitis syndrome (CPS). The study was performed by V. Smelov and colleagues from St. Petersburg, Russia, and published in the November, 2004 issue of European Urology. A population of 304 men aged 19 to 54 (mean 28 years) with lower urinary tract symptoms (LUTS) compatible with the diagnosis of CPS associated with a positive urethral and prostatic fluid culture of C. trachomatis comprised the study group. The absence of other organisms such as Trichmonas vaginalis, gonococci and genital mycoplasma was confirmed by urethral swab and EPS (expressed prostatic secretion) culture. The in vitro activity against chlamydia was tested for the four flouroquinolones: ofloxacin, ciprofloxacin, pefloxacin and lomefloxacin as well as for doxycycline and azithromycin. Results showed that the most active agent was azithromycin, followed by ofloxacin, pefloxacin, lomefloxacin and ciprofloxacin. The least active agent among the antibiotics tested was doxycycline. The authors postulate that the widespread use of doxycycline may have contributed to a high level of resistance to this antibiotic within this patient population. In conclusion, the authors report on the activity of multiple antibiotic agents against Chlamydia trachomatis isolates from men with chronic prostatitis syndrome. The results suggest that azithromycin and ofloxacin show the best in vitro activity against this organism. The authors also suggest that ofloxacin may be the treatment of choice for patients being treated for bacterial prostatitis and chronic prostatitis syndrome because of its activity against other common bacterial isolates as well as against the less common chlamydial agent.
Tillbaka till sidan Bakteriologisk diagnostik
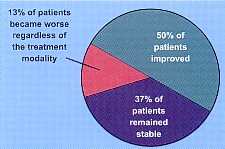
Sequential monotherapy yields poor results in CPPS, Canada Dr. Nickel Urology Times Urology Times® Vol. 32, No. 10 _ July 2004 From http://www.urologytimes.com The Leading News Source for Urologists Penny
Allen, UT CORRESPONDENT, San Francisco. First-line alternatives One-hundred consecutive CP/CPPS patients (age range, 20 to 70 years) were enrolled in the study from 1999 to 2000. All had refractory CP/CPPS and had been referred to the clinic by other urologists. Each patient was approached with a sequential monotherapy strategy. If treatment was successful, patients continued with that treatment. If unsuccessful, treatment was discontinued and a new therapy was instituted. Patients were followed for 1 year. The first-line therapeutic alternatives were alpha-blockers, anti-inflammatory medications, and prostate massage, based on whether the patient’s major symptoms were voiding symptoms, pain, or copious expressed prostatic secretions. Antibiotic therapy was not one of the first-line therapies. But the few patients who had not received antibiotics before or who had shown previous response did receive an initial 6 weeks of a fluoroquinolone antibiotic. That’s because a 50% response rate is seen, even when cultures are negative, Dr. Nickel explained. After 6 to 12 weeks, the patients were switched to one of the other primary therapies or to one of the secondary therapies, which included finasteride (Proscar), pentosan polysulfate (Elmiron), phytotherapy with quercetin (Prosta-Q), and various types of physical therapy. Overall, the reduction in scores on the National Institutes of Health’s Chronic Prostatitis Symptom Index were statistically significant for 71% of the patients. But that figure is misleading, Dr. Nickel explained. Just over one-third (37%) of the patients had an improvement that was “clinically perceptible” - a 25% decrease in total symptom score. And only 19% had a “clearly significant” improvement, defined as a decrease of 50% or more in total symptom score. Monotherapy vs. multimodal
Zabkowski T, Peterek J, Stawarz B, Bejm J, Sulik M, Bancer M liniki Urologii Centralnego Szpitala Klinicznego Wojskowej Akademii edycznej w Warszawie. More than 25% of patients who declare indisposition of the urinary tract suffer from prostate infection. Progress in the me-dical treatment of this type of infection has been achieved largely due to the introduction of new sorts of antibiotics and deve-lopment of modern diagnostic methods. The aim of the study is to determine the causes of prostate infections. A bacteriological examination of the prostate secretion in 28 patients after "per rectum" massage were conducted in the Urology Clinic of the Central Clinical Hospital of Military Academy in Warsaw from March 1995 to September 1997. All the patients had previously undergone medical treatment and long-term pharmacotherapy. A high percentage of fungal infections as well as the increased occurrence of Chlamydia trachomatis have been observed. PMID: 10628269, UI: 20093756 http://www.urol.com
Rodney U. Anderson, Christine Chan, Stanford, CA; Timothy Sawyer, Los Gatos, CA; David Wise, Sebastopol, CA This team evaluated a new approach to treatment of CPPS with the Stanford University-developed protocol of physical therapy (myofascial muscular release) directed mainly at the pelvic floor in conjunction with a cognitive behavioral therapy called paradoxical relaxation. In this type of relaxation training, patients focus on their tension, yet try to relax from it. The team treated 138 men with CPPS not helped by other treatments with this approach as the only therapy for at least one month. Patients had physical therapy weekly and had individual instruction in the relaxation technique weekly for up to 8 weeks with a recommendation for daily home practice with instructional audiotapes. The team assessed how the men were doing with the NIHCPSI, a Pelvic Pain Syndrome Survey (PPSS), and the Global Response Assessment (GRA) questionnaire. More than half of patients treated with this protocol had clinical improvements and a 25 % or better decrease in pain and urinary symptom scores assessed by the PPSS. Among men who had at least 50% improvement, median scores decreased 69% for pain and 80 % urinary symptoms. Both scores decreased significantly by a median of 8 points when the 25 %-or-better improvement was first seen. After a median of five treatments, GRA scores improved moderately or markedly for 72 % of patients. Both the PPSS and NIH-CPSI scores showed similar levels of improvement after treatment. The median pretreatment NIH-CPSI total score of 24 decreased significantly-by a median of 11 points (46 %) for patients who were markedly improved and by 8 points (24 %) for those who were moderately improved. The researchers believe their study shows that this therapeutic protocol can give men with CPPS pain and urinary symptom relief comparable with that of traditional therapy. För mer information se http://www.pelvicpainhelp.com/
In a study done by John Krieger et al and published in the Journal of Clinical Microbiology, Volume 34, Number 12, December 1996, Prokaryotic DNA Sequences in Patients with Chronic Idiopathic (non- bacterial) Prostatitis. They reported that 87% of men included in this study diagnosed as having non-bacterial prostatitis by Meares-Stamey culture procedure were found to have bacterial prostatitis by using PRC (polymerase chain reaction) and DNA analysis method. The 135 patients selected for study underwent prostatic biopsy. The biopsy needle was introduced through a larger needle that penetrated the skin first, avoiding contamination from the skin flora. The study found that 77% have bacterial DNA in their prostate biopsy specimens when they are tested for bacterial DNA using the PCR. An additional 10% of the 135 patients had Mycoplasma, Chlamydia or Trichomonas. Five had M. genitalium, 4 had C. trachomatis. 2 had T. vaginalis, and 1 had both M. genitalium and C. trachomatis. Ten patients were positive for one or more of the specific organisms mentioned above. Other organisms reported were Vibrio furnissii, Staphylococcus aureus. Staphylococcus epidermidis. Escherichia coli, and Aeromonas allosaccharophilia as possible etiologic agents in chronic non-bacterial prostatitis. Patients typically exhibited more than one kind of 16SrRNA, implying infection from more than one kind of organism. Of the patients, 103 were positive for 16SrRNA, indicating that the majority of the 135 patients tested may have more than one organism involved. Of the 120 patients 30 were positive for tetM- tetO-tetS. Of these 30, 29 were also positive for 16SrRNA. Krieger et al wrote that half of all men experience symptoms of prostatitis at some time in their lives and the mean age of their subjects was 38.3 years. This indicates that probably 1.5 billion men will suffer from symptomatic prostatitis. This does not include asymptomatic men with pus cells in the EPS but with normal size prostate by digital rectal examination (DRE). This study indicated that more than 87% of men with bacterial prostatitis, diagnosed as non bacterial, will not be treated with antibiotics but may accept remedial measures to relieve symptoms. These measures in most cases are not successful and the cases will eventually be classified as prostatodynia. In the accepted standard of diagnosing prostatitis, only 10% will be classified as bacterial. These men will be given weeks of target antibiotics which will only cure 30% of them. It took five years to complete this study and it only confirmed the hypothesis that I have followed. The presence of pus cells in the expressed prostatic secretion (EPS) means infection important enough to treat whether the patient has symptoms or not. Bacterial DNA found in prostatic biopsy is an indication of infection of the prostate due to bacteria. The finding that multiple organisms are involved in some patients with chronic prostatitis supports and justifies the multiple antibiotics therapy. The use of single antibiotics given for weeks and months results in treatment failure in over 80% of cases. Hela rapporten finns på http://web.idirect.com/~ino/main.htm
Statistikinformation från BPSA (The British Prostatitis Support Association) Although the name prostatitis means inflammation of the prostate gland, the disease is more usefully regarded as prostatitis syndromes (ref JCN P1). It affects men of all ages almost equally, with a slight bias to the young (11.5% 20 to 50, 8.5% over 50 - ref 2, 2a) - is the most common urological problem diagnosed in men under the age of 50, and third most common for men over 50. Two studies were obtained in an independent literature search. One of them, appearing in the March issue of The Journal of Urology, placed the prevalence of the disease at 11.5% in men between 20 and 50 years old and 8.5% in men aged 50 and older (J Urol 2001; 165:842-5) An earlier study used Olmstead County data to obtain an overall prevalence rate of 9% (Urology 1998; 51:578-84). The initial study data was presented at the annual AUA meeting in Anaheim." "...11% men had a ...diagnosis of prostatitis....14% of fit men had a previous diagnosis of prostatitis....2 to 6% of men.... are experiencing prostatitis-like symptoms at any particular time." (ref JCN P3) ISOPs kommentar: Ovanstående är ett utdrag från en korrespondens mellan BPSA och det brittiska radio- och TV-bolaget BBC. Med JCN avses en bok om prostatit författad av Professor J. Curtis Nickel, Canada (se sidan "Litteratur m.m "), "The prostatitis manual", ISBN 1-904218-08-3, Bladon Medical Publishing, 116 pages (tel 01608 644436) (£25).
Journal of Urology 1999; 161 (4 suppl):32 Abstract 111. International population-based study of urological conditions: The Urepik Study II. Comperative prostatitis data. Robertson C, Boyle P, Nonis A et al. An interesting study comparing the United Kingdom, France, the Netherlands and Korea found that 5-10 % of men have prostatitis symtoms, with highest prevalence in France.
ALZA Corporation, pressmeddelande 00-02-15, USA In
the urology setting, ALZA (ett stort amerikanskt läkemedelsföretag) will be
supporting studies to explore the role of Elmiron in the treatment of
chronic pelvic pain syndrom, or non-bacterial prostatitis, a condition that
affects between
Prevalence of Prostatitis-like Symptoms in Lenox and Addington (L&A) County, Canada. JC Nickel, D Hunter, J Downey, J Clark. Queen's University, Kingston, Canada Results: The study is ongoing. At time of interim analysis (September 15, 1999), 803 men had completed the survey. Seventy-five (9.3%) of the men were identified as having chronic prostatitis-like symptoms. As well as perineal or ejaculatory pain and discomfort, 60 % of the prostatitis group also had pain/discomfort in the pubic or bladder area. The average NIH-CPSI pain score for prostatitis group was 8.6 0.3. The average age (years) of the prostatitis population was 51 compared to 52 for men without prostatitis-like symptoms.
Chronic Prostatits Workshop Bethesda, USA November 1999, Dr. Aare Mehik, Finland. We studied whether prostatitis is more prevalent for Finns. Until recently the attitude in Finland was what is not killing patients is not important. We started a cross-sectional study in 1993 -1994, where we asked 102 questions. There were 2,500 randomly chosen respondents, of whom we got answers from1832. We then called non-respondents. We found a total of 261 chronic prostatitis patients. Of the respondents, the rate of prostatitis is 14 per cent. In our study, of these patients, 21.3 per cent suffer problems at least once a year. Fifty-eight per cent thought the main reason is cold climate and winter. They said they suffered in winter and not in the summer. [Maybe some respondents had BPH] Aare Mehik, MD Department of Surgery/Division of Urology Oulu University Hospital Kajaanintie 50 Oulu 90220 Finland Tel: 358-8-315-2011 Fax: 358-8-315-2447, E-mail: amehik@cc.oulu.fi
Prevalance of prostatitis-like symptoms (PS) in a population-based study, Singapore, 1999 James Khiaw-ngiap Tan*, Damian J Png, Lewis C Liew, Man-Kay Li, Kesavan Esuvaranathan, Mee-Lian Wong, National University of Singapore, Singapore. A population-based cross-sectional survey was conducted in Singapore in 1999 to evaluate 'prostatitis-like symptoms', lower urinary tract symptoms (LUTS) and erectile dysfunction (ED). PS was defined as pain or discomfort in the perineum, testicles, tip of penis or bladder/suprapubic region in association with LUTS and impaired quality of life (QoL). Questions similar to the National Institutes of Health Chronic Prostatitis Symptom Index were used. Altogether, 845 males aged 21 to 70 were evaluated. Although a significant proportion of respondents have LUTS in our largely Chinese population, only 2.5% have prostatitis-like symptoms. This is contrary to others' reports (Nickel's 6-8%, Mehik's 14.2%). Those having PS have a significantly worse erectile function and quality of life score but no difference in the level of anxiety. More subjects have impaired QoL due to their LUTS than due to prostatitis-like symptoms which were much less common
The prevalence of chronic prostatitis-like symptoms in young men: a community-based survey. Military Manpower Administration, Taejeon, Korea. Ku JH, Kim ME, Lee NK, Park YH. randyku@medigate.net We surveyed the prevalence of chronic prostatitis-like symptoms in young men using the National Institutes of Health (NIH) Chronic Prostatitis Symptom Index (CPSI) and determined the clinical validity of the NIH-CPSI among men in the community. Of 29,017 men aged 20 years dwelling in the community, 8,705 men were randomly selected at a 30.0% sampling fraction and a total of 6,940 men (a response rate 79.7%) completed a selfadministered questionnaire. Six percent reported having pain or discomfort in more than one area . About 5% did not feel that the bladder emptied fully after urinating more than 1 time in 5 and 10.5% had to urinate again within 2 h more than 1 time in 5. As the scores for pain or discomfort increased, those for urinary symptoms and impact on quality of life increased (P 0.001; Armitage test). As the scores for urinary symptoms increased, those for pain or discomfort and impact on quality of life also increased (P 0.001; Armitage test). The communitybased prevalence of chronic prostatitis-like symptoms were found to be high in young men as well as in older men. Our findings indicate that men with pain or urinary symptoms experience a negative impact on their quality of life and the NIH-CPSI provides a valid measure for the general population.
Vi redovisar här statistik på hur den procentuella åldersfördelningen är på de som kontaktat oss (via e-mail, telefonsamtal och genom brev) och som är drabbade av kronisk prostatit. Av större statistiskt intresse är givetvis vid vilken ålder som sjukdomen manifisterade (blev tydligt märkbar hos den drabbade), men vi har tyvärr inget underlag för att kunna göra en sådan redovisning. Drabbade under 20 år: cirka 2 % Drabbade 20-40 år: cirka 50 % Drabbade 40-60 år: cirka 28 % Drabbade äldre än 60 år: cirka 20 %
Milstolpar i försöken att finna orsaken till kronisk prostatit. 1800s: Causes include chilling, sexual indulgence, alcoholic drink, violent exertion, injury, horseback and bicycle riding. (Does any of this sound familiar?) 1913: Prostatic fluid rigorously cultured. (How did "we" forget how to do this?) 1926: Role of bacteria in chronic prostatitis confirmed. (Not "all" CP evidently). 1927: Importance of streptococci and staphylococci. (I guess "we" forgot this too). 1928: Retrograde infection secondary to patient prostatic ducts (What does this mean?) 1930: Landmark study of prostatic fluid cultures (Also forgotten?) 1938: Intestinal tract source of bacteria (Proven or merely suggested?) 1943: Chronic bacterial prostatitis result of acute or subacute prostatitis (Really? I have been told that acute bacterial prostatitis is simply a different disease. Does it really progress to chronic?). 1957: Inflammation may exist as a non-bacterial process (43 years ago! What have "we" been doing since?) John Garst (professor emeritus) garst@chem.uga.edu
Historical perspective of prostatitis The prostate gland was described in the anatomical studies of Herophilus about 350 BC and was rediscovered in the 16th century by the Venetian physician Nicola Massa. At the same time the physician Riolanus noted that bladder obstruction can be caused by swelling of the prostate gland. Prostatitis as a clinical entity/syndrome was first described in 1815 by Legneau, who noted that inflammation of the prostate gland could be a complication of urethritis (von Lackum 1928). The first accurate description of the pathology of prostatitis in written form was presented by Verdies in 1838, and this was later confirmed and updated by Hugh Young, Gereghty and Stevens in 1903 and published in 1906 (Young et al. 1906, von Lackum 1928). The time between the 1880 and 1928 was a period of searching for bacteria and confirming the postulates of Koch and Wirchow related to the mechanisms of bacterial infections acting in the human body (Hitchens & Brown 1913, von Lackum 1927). Between 1900 and 1930, the basic chemistry of prostatic fluid was studied and the role of possible pathogen bacteria cultured from the prostate gland and from prostate secretion was defined and von Lackum´s theory of possible retrograde secondary infection ascending from the urethra to the prostatic ducts was clinically demonstrated by several physicians (Young et al. 1906, Hitchens & Brown 1913, von Lackum 1927, Nickel 1930). The period between 1930 and 1960 was marked by an active search for aetiological factors related to prostatitis syndrome, factors that could be responsible for its chronicity and the histological changes that take place, fibrosis and scarring together with late functional disorders of the prostate gland. Despite of all these new findings, there were many internists and psychoanalysists who denied the existence of chronic prostatitis processes, and the latter group termed such symptoms ”anal/rectal psychoses” (Cumming & Chittenden 1938). Ritter and Lippow (1938) searched for an explanation for the natural history of the pathological processes involved in prostatitis, and they also described the histological findings during acute phase of inflammation as hyperaemia, oedema, cellular infiltration of polymorphonuclear leukocytes and round cells in the prostate tissue. Grant (1938) noted that the infection was mostly located in the ducts and acini of the prostate. On the other hand, Kretschmer (1937) drew conclusions from 1000 cases that pointed to polyaetiological aspects of the disease, and also reflected on the sexual life of patients. There was a period in the 1940s and 1950s when it was generally accepted that an important offending organism in cases of acute infectious prostatitis was gonococcus. Henline (1943) reported that untreated gonococcal urethritis was a possible aetiological factor in over 20–30% of cases of chronic prostatitis symptoms, but Kretschmer (1937) found gonococcus to be an aetiological reason for prostatitis in only 2.4% cases. Genitourinary tuberculosis was regarded as a specific aetiological factor between 1900 and 1960. Tuberculosis of the prostate gland as only affected genital organ was found in 12% cases in an autopsy series, and the majority of patients with upper genitourinary tuberculosis were also found to have signs of prostatic irritation (Moore 1937, Meares 1998). In the late 1950s it was recognized and noted, especially by Campbell (1957), that chronic prostatitis may be present in the prostate gland without any clinical symptoms, and it was also realized that a disease such as prostatitis can be congestive and non-bacterial. The active clinical research period of the 1970s and 1980s, was motivated by the findings of Meares and Stamey (1968), which pointed to a new direction in the diagnosis of prostatitis, and those of Drach et al. (1978), which provided a new classification of the disease. This was followed by a period of collecting clinical experience and basic knowledge on prostatitis at large, using new laboratory methods for bacterial cultures, microscopy and immunofluorescence imaging. From the 1990s onwards a young generation of disappointed urologists who did not accept all the written data from past concerning prostatitis as a forgotten ”light urological ambulatory pathology” and ”not needing special urological care” started a new era in prostatitis research (Nickel 1999, Nickel et al. 1999b). Ovanstående artikel finns på http://herkules.oulu.fi/isbn9514265068/html/index.html. Aare Mehik, MD. Department of Surgery/Division of Urology Oulu University Hospital Kajaanintie 50 Oulu 90220 Finland Tel: 358-8-315-2011 Fax: 358-8-315-2447, E-mail: amehik@cc.oulu.fi Ovanstående artikel finns också för utskrift i pdf-format på en A4 sida
Ovanstående ”belyser” bl.a. att sjukdomarna är betydligt vanligare än man tror!
Tillbaka till Förekomsten (prevalensen) av prostatit (På sidan Prostatasjukdomar)
|